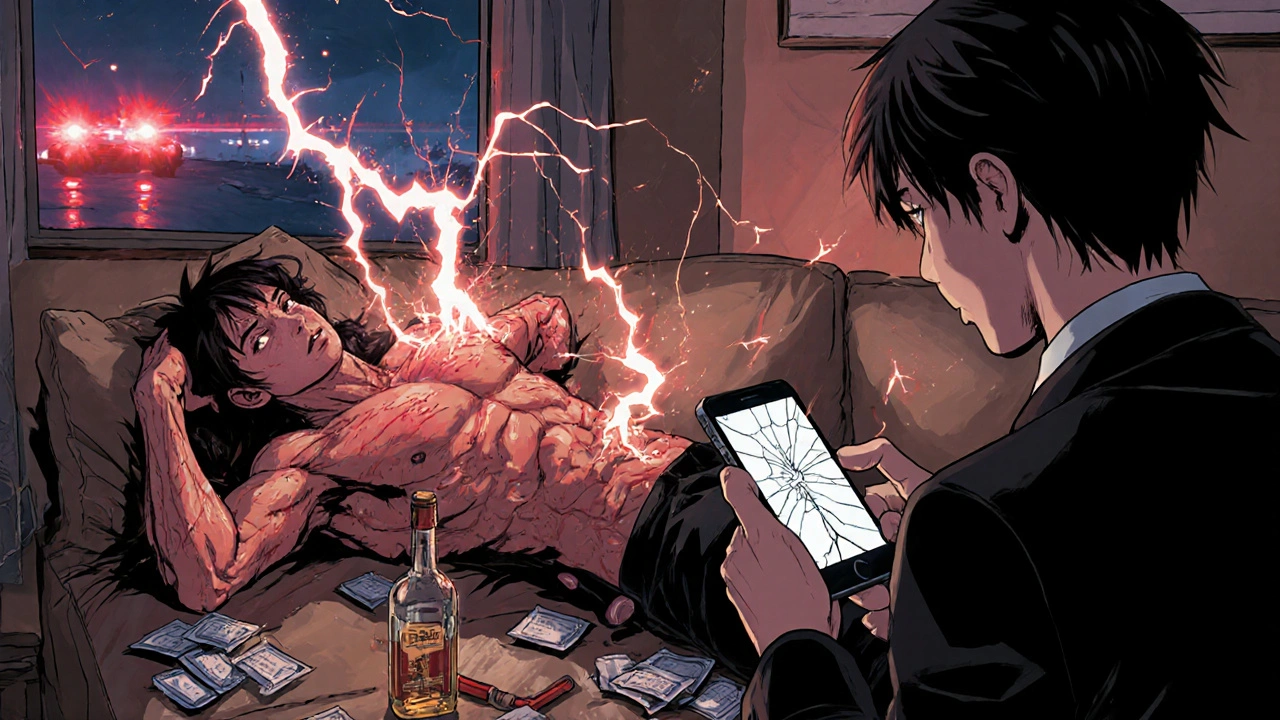
Every year, tens of thousands of people die from medication overdoses - not because they wanted to end their lives, but because they didn’t know what was happening until it was too late. A person might take an extra pill for pain, mix a prescription with alcohol, or unknowingly swallow a counterfeit pill laced with fentanyl. In minutes, their breathing slows, their skin turns blue, and their body shuts down. The difference between life and death often comes down to recognizing the signs early - and acting fast.
What Happens During a Medication Overdose?
A medication overdose isn’t just taking too much of a drug. It’s when your body can’t process what you’ve taken, and your brain and organs start to fail. This can happen with prescription painkillers, sleep aids, anxiety medications, stimulants, alcohol, or even common over-the-counter drugs like acetaminophen. The most dangerous cases involve synthetic opioids like fentanyl, which is 50 to 100 times stronger than morphine. Just two milligrams - about the size of a few grains of salt - can kill someone who isn’t used to it.Overdose doesn’t always look like someone passed out on the floor. Sometimes, the person is awake but unresponsive. They might be confused, slurring words, or staring blankly. Their breathing might be slow - less than 10 breaths per minute - or irregular, with long pauses between breaths. In opioid overdoses, their pupils become tiny pinpoints. In stimulant overdoses, they might be sweating, shaking, or having seizures. The key is knowing that medication overdose signs aren’t always obvious, and waiting to see if they “sleep it off” can be fatal.
Common Signs Across All Types of Overdose
No matter what drug is involved, there are warning signs that signal an emergency:- Unresponsiveness - shaking them, calling their name, rubbing their sternum - if they don’t react at all, it’s a red flag.
- Slow, shallow, or stopped breathing - if there’s more than 10 seconds between breaths, their brain is starving for oxygen.
- Blue or gray lips and fingernails - this means oxygen levels are dangerously low.
- Choking or gurgling sounds - often mistaken for snoring, this is a sign they’re struggling to breathe and may vomit.
- Pale, cold, clammy skin - their body is going into shock.
- Extreme drowsiness or inability to stay awake - not just tired. They can’t be roused.
- Vomiting while unconscious - this is especially dangerous with alcohol or depressants, as they can choke on their own vomit.
These symptoms don’t always show up together, but if you see even two or three, don’t wait. Call for help immediately.
Drug-Specific Overdose Symptoms
Different drugs affect the body in different ways. Knowing the patterns can help you respond faster.Opioids (fentanyl, heroin, oxycodone, morphine)
Opioid overdoses are the leading cause of drug-related deaths in Australia and the U.S. The classic signs - known as the “opioid triad” - are:
- Pinpoint pupils (so small they look like dots)
- Unconsciousness or inability to wake up
- Slow or stopped breathing (less than 12 breaths per minute)
People may also have a limp body, snoring or gurgling sounds, and cold, bluish skin. The risk spikes after someone has been away from the drug for a while - like after detox or jail - because their tolerance drops fast. A dose they used to handle can now kill them.
Stimulants (cocaine, methamphetamine, Adderall)
Unlike opioids, stimulant overdoses don’t make people sleepy. Instead, they overheat and go into cardiac crisis:
- High body temperature (over 40°C / 104°F)
- Fast, irregular heartbeat or chest pain
- Severe headache or dizziness
- Agitation, paranoia, hallucinations
- Seizures
People might be sweating profusely, yelling, or acting violently. Their skin may be hot and dry. This type of overdose can cause heart attack, stroke, or organ failure within minutes.
Depressants (alcohol, benzodiazepines, barbiturates)
These drugs slow everything down - including breathing and heart rate. Signs include:
- Slurred speech
- Loss of coordination, stumbling
- Confusion or memory loss
- Vomiting while unconscious
- Slow, irregular breathing
Alcohol poisoning is a form of depressant overdose. If someone drinks too much and passes out, they’re at risk of choking, hypothermia, or respiratory arrest. Never leave someone who’s passed out alone.
Polysubstance Overdose (mixing drugs)
Most overdoses today involve more than one substance. Fentanyl is often mixed into cocaine, meth, or counterfeit pills without the user’s knowledge. In 2022, over half of all overdose deaths involved multiple drugs. Symptoms can be confusing - someone might have pinpoint pupils (opioid) and a racing heart (stimulant) at the same time. This makes it harder to guess what’s happening - but the response is the same: call for help immediately.
What to Do If You Suspect an Overdose
Time is everything. The average person dies within 1 to 3 minutes after their breathing stops. Here’s what to do:
- Call emergency services - in Australia, dial 000. In the U.S., dial 911. Don’t wait. Don’t text. Call.
- Check breathing - if they’re not breathing or breathing very slowly, start rescue breathing: tilt their head back, pinch their nose, give one breath every 5 seconds.
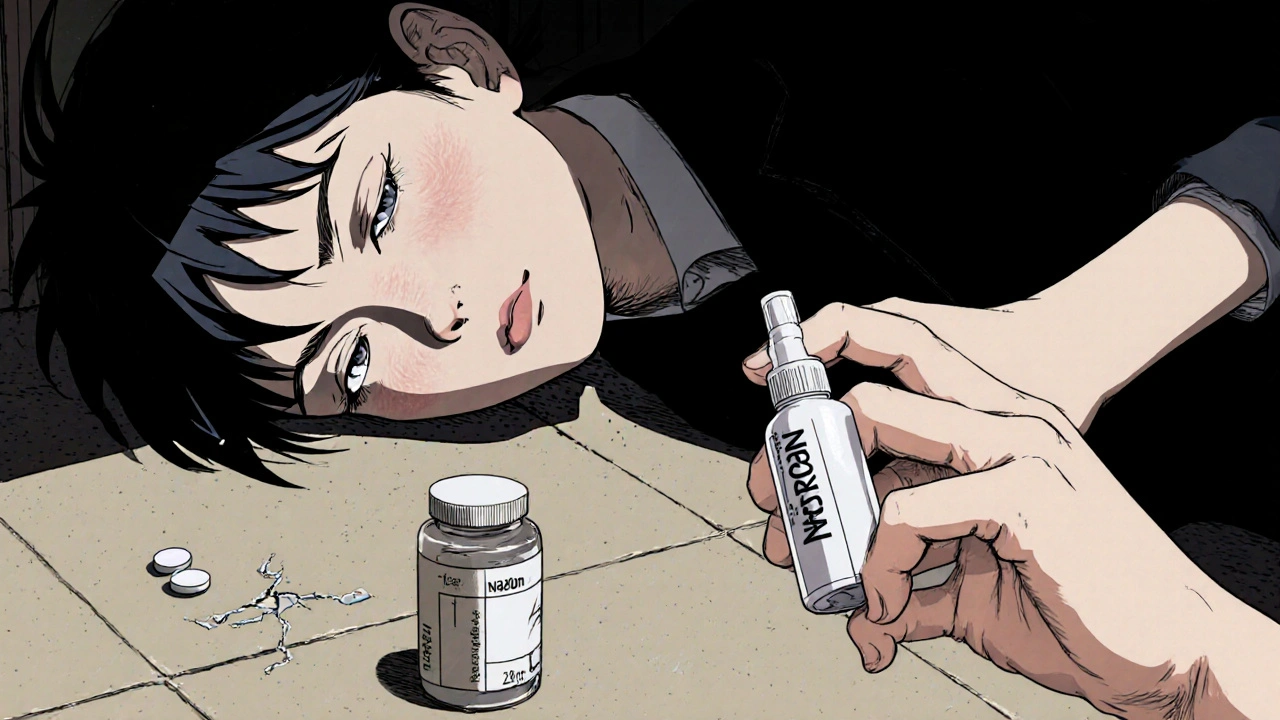
- Administer naloxone if available - naloxone (brand name Narcan) reverses opioid overdoses. It’s safe, even if you’re not sure it’s an opioid overdose. Use the nasal spray: one spray in each nostril. You can give a second dose after 2-3 minutes if there’s no response.
- Place them on their side - the recovery position prevents choking if they vomit.
- Stay with them - even if they wake up, they can relapse into overdose. Wait for paramedics.
Never try to make them walk, give them coffee, put them in a cold shower, or let them “sleep it off.” These myths cost lives. In 29% of fatal overdoses, people waited too long because they thought the person would wake up on their own.
How to Prevent Overdose
Prevention isn’t just about avoiding drugs - it’s about reducing risk if you or someone you know uses them.
- Use fentanyl test strips - these cheap, easy-to-use strips can detect fentanyl in powder or pills. If it’s positive, don’t use it. Or use with someone else present, and have naloxone ready.
- Never use alone - overdoses are less likely to be fatal if someone is there to help. Use with a friend, or call someone while you use.
- Start low, go slow - if you haven’t used in a while, your tolerance is lower. Use half the dose you used to.
- Don’t mix drugs - especially alcohol with opioids or benzodiazepines. This combination is deadly.
- Carry naloxone - it’s now available over the counter in pharmacies without a prescription. Keep it in your bag, your car, your home. It saves lives.
Many people think overdose only happens to “other people.” But it doesn’t discriminate. It can happen to someone with a prescription, someone using recreationally, or someone who bought a pill thinking it was Xanax - but it was fentanyl.
Where to Get Help
If you’re worried about your own use, or someone else’s, help is available. The Alcohol and Drug Foundation offers free, confidential advice. In Australia, call 1800 250 015. In the U.S., call SAMHSA’s National Helpline at 1-800-662-4357. It’s 24/7, free, and no judgment.
Pharmacies across Australia now stock naloxone without a prescription. Ask for it. Learn how to use it. Keep one at home. It’s not a sign of failure - it’s a sign of care.
Overdose doesn’t have to be a death sentence. It’s preventable. Recognizing the signs, acting fast, and having naloxone nearby can mean the difference between someone going home - or not.



Ryan Everhart
November 12, 2025 AT 11:16David Barry
November 13, 2025 AT 03:15Alyssa Lopez
November 13, 2025 AT 03:52edgar popa
November 13, 2025 AT 14:08seriously. do it.
Eve Miller
November 13, 2025 AT 18:38Chrisna Bronkhorst
November 14, 2025 AT 03:11Deepa Lakshminarasimhan
November 15, 2025 AT 16:58Erica Cruz
November 17, 2025 AT 07:34Johnson Abraham
November 18, 2025 AT 22:32also why is everyone so scared of fentanyl? its just a pill. if you can't handle it, dont be a wuss.
lol #fentanylisafad