More than half of all asthma cases are allergic asthma - a condition where your immune system overreacts to harmless things like pollen, dust mites, or pet dander. It’s not just about sneezing or itchy eyes. When these allergens get into your airways, they trigger inflammation, tightening of the muscles around your bronchial tubes, and mucus buildup. The result? Wheezing, shortness of breath, chest tightness - and sometimes, emergency visits.
What Makes Allergic Asthma Different?
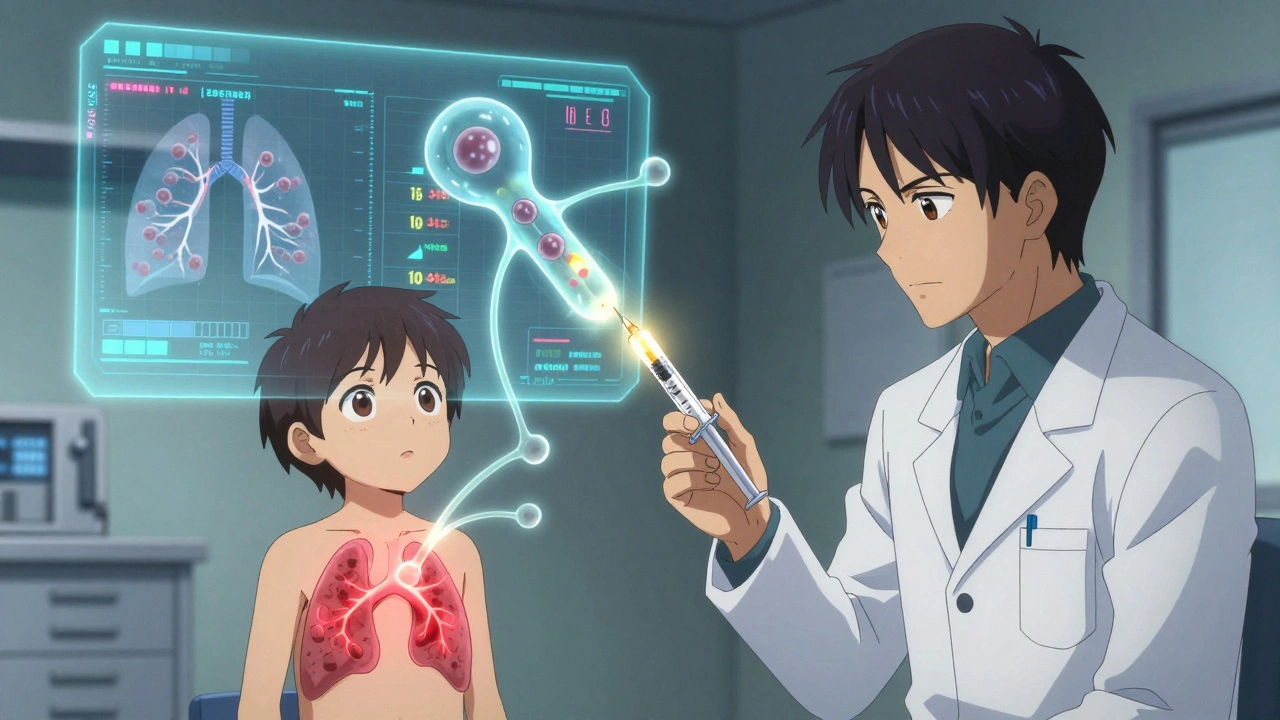
Allergic asthma isn’t just asthma with allergies. It’s asthma driven by a specific immune response involving IgE antibodies. When you breathe in an allergen, your body treats it like an invader. Mast cells release histamine and other chemicals, attracting eosinophils - inflammatory cells that swell your airways. This isn’t random. Blood tests often show IgE levels above 100 kU/L, and skin prick tests will show clear wheals (raised bumps) when exposed to triggers like cat dander or ragweed.
Unlike non-allergic asthma, which often starts in adulthood and is linked to stress, cold air, or pollution, allergic asthma usually begins in childhood. Studies show 80% of kids with asthma have it, and 60% of adults do too. Family history matters: if a parent has allergic asthma, your risk jumps threefold. The good news? Because the triggers are identifiable, you can target them directly - something you can’t always do with other asthma types.
Top Triggers and When They Hit Hard
Not all allergens act the same. Some are year-round. Others explode seasonally.
- Tree pollen (February-April): Peaks in March. In Sydney, eucalyptus and cedar can be major offenders. Pollen counts above 10 grains/m³ can trigger symptoms.
- Grass pollen (May-July): June is the worst month. Ryegrass is a big one in Australia. Counts can hit 100 grains/m³ on windy days.
- Ragweed (August-October): Less common in Australia than the U.S., but still present in some regions. Peak in September.
- Dust mites: These microscopic bugs live in bedding, carpets, and upholstered furniture. They thrive where humidity is above 50%. Homes with humidity over 60% often have dust mite levels above 2 µg/g - the threshold that triggers reactions.
- Cat dander (Fel d 1): Even if you don’t own a cat, 79% of U.S. homes have detectable levels. In Australia, cat ownership is high, making this a major trigger. Levels above 8 µg/g in dust are enough to cause symptoms.
- Mold spores (Alternaria): Especially dangerous after thunderstorms. When spore counts exceed 500/m³, ER visits for asthma spike by 3.5 times.
Real-world impact? A 2023 survey of 2,850 asthma patients in the UK found 41% had at least one ER visit during high pollen season - even while taking their prescribed meds. That’s not failure of medication. It’s failure of trigger control.
How to Avoid Allergens - The Proven Steps
Avoidance isn’t about living in a bubble. It’s about smart, measurable changes.
Bedding and Indoor Air
- Use allergen-proof mattress and pillow covers (look for a pore size under 10 microns). Brands like AllerZip Pro work - but any certified cover does.
- Wash bedding weekly in water hotter than 130°F (54°C). Cold water doesn’t kill dust mites. This cuts allergen levels by 90%.
- Keep indoor humidity between 30-50%. Use a hygrometer to monitor. A dehumidifier like the AprilAire 500M can drop mite levels from 20 µg/g to under 0.5 µg/g.
- Vacuum twice a week with a HEPA-filter vacuum. Standard vacuums just blow allergens back into the air. A Dyson V15 or similar reduces cat allergen by 42%.
Pollen and Outdoor Exposure
- Check daily pollen forecasts. The National Allergy Bureau and apps like Pollen.com show real-time counts. Stay indoors when tree or grass pollen exceeds 9.7 grains/m³.
- Keep windows closed during high pollen days - especially at night. Air conditioning helps, but only if filters are clean.
- Wear an N95 mask when mowing the lawn, raking leaves, or gardening. It cuts pollen exposure by 85%.
- Shower and change clothes after being outside. Pollen sticks to hair and clothes. One 2021 study found this reduces allergen transfer to bedding by 70%.
Cats and Pets
If you’re allergic to cats, you don’t need to give yours up - but you need to manage it.
- Keep cats out of the bedroom. This is the single most effective step.
- Bathe your cat weekly. It reduces Fel d 1 levels by 30-50%.
- Use a HEPA air purifier in the living area. Look for one with a CADR rating over 300 for your room size.
Immunotherapy: The Only Treatment That Changes the Course
Medications - inhalers, antihistamines, steroids - manage symptoms. But immunotherapy is the only treatment that can actually change how your immune system responds to allergens.
There are two types: subcutaneous (SCIT - allergy shots) and sublingual (SLIT - tablets or drops under the tongue).
Allergy Shots (SCIT)
- Start with weekly injections over 4-6 months, slowly increasing the allergen dose.
- Once you reach the maintenance dose (usually 0.5 mL of 1:10,000 concentration), you get shots every 2-4 weeks for 3-5 years.
- 70-80% of people see significant improvement after 12-18 months.
- Benefits last years after stopping - unlike daily meds that stop working when you skip a dose.
- Side effects? Minor swelling at the injection site. Serious reactions are rare (less than 0.1% per injection).
Sublingual Immunotherapy (SLIT)
- Daily tablets or drops - no needles.
- Grastek (for grass) and Odactra (for dust mites) are FDA-approved. In Australia, SLIT is available under prescription.
- Reduces asthma symptoms by 35% in dust mite-allergic patients, compared to 15% with inhaled steroids alone.
- Downside? Oral itching or throat irritation in the first month - common, but usually fades.
- 35% of people quit because of this, but sticking through the first 3 months makes a big difference.
According to a 2021 Cochrane review of over 12,000 patients, immunotherapy reduces asthma medication use by up to 40%. Long-term, it can cut the risk of developing new allergies by 50%.
Who Should Skip Immunotherapy?
Not everyone with allergic asthma is a candidate.
- If your asthma is poorly controlled - you’re still having daily symptoms or needing rescue inhalers - start with medication first. Immunotherapy can trigger a flare if your airways are too inflamed.
- If you have severe heart disease or are on beta-blockers, shots aren’t safe.
- And here’s a big one: not all asthma labeled ‘allergic’ actually is. About 30% of patients diagnosed with allergic asthma based on symptoms have non-type 2 inflammation. These patients won’t respond to biologics or immunotherapy. Blood tests for eosinophils (>300 cells/µL) and FeNO (>25 ppb) help confirm true allergic asthma.
Don’t spend $30,000 a year on a biologic if your asthma isn’t driven by IgE. Get tested first.
What’s New in 2025?
Technology is making management smarter.
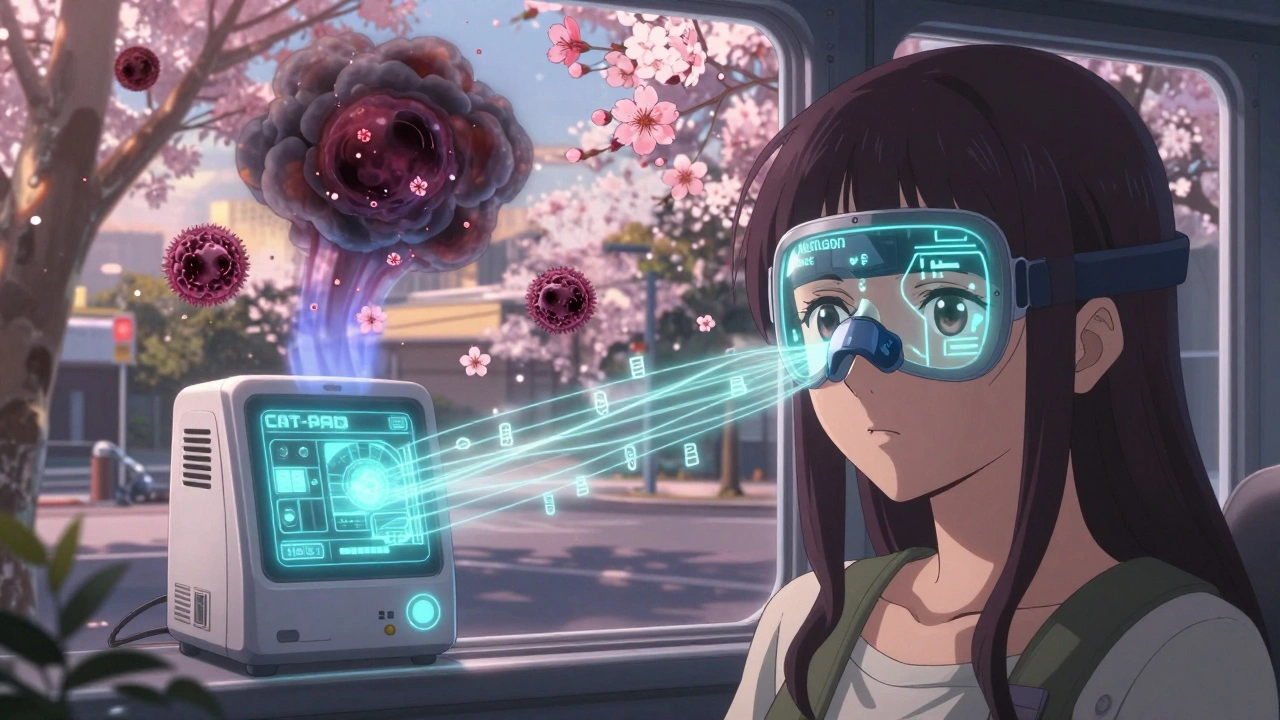
- The Allergen Insight nasal sensor (FDA breakthrough in 2023) detects airborne allergens as low as 0.1 µg/m³ and alerts your phone. It’s still expensive, but pilot programs in Sydney schools are showing promise.
- AsthmaIQ, launched in April 2024, uses AI to combine pollen forecasts, your inhaler use, and weather data to predict your next flare-up - with 92% accuracy.
- New peptide immunotherapy for cat dander (CAT-PAD) cuts the build-up phase from 6 months to just 8 weeks.
- Research is now using genetic markers (like the GSDMB gene) to predict who will respond best to immunotherapy - with 85% accuracy.
One 12-year-old in the U.S. with severe cat allergy went from wheal sizes of 15mm on skin tests to negative after 3 years of immunotherapy. His IgE dropped from 120 kU/L to 15 kU/L. He no longer needs daily meds. That’s not just symptom control. That’s disease modification.
When to See an Allergist
If you’re using your rescue inhaler more than twice a week, or if you’ve had an asthma attack that needed emergency care - it’s time to see a specialist.
An allergist can:
- Confirm if your asthma is allergic with skin or blood tests
- Identify your exact triggers (not just ‘pollen’ - but which type)
- Recommend personalized avoidance strategies
- Prescribe immunotherapy if you’re a candidate
- Monitor your IgE and eosinophil levels over time
Don’t wait until you’re in the ER. Allergic asthma is one of the few chronic conditions where you can actually reduce your risk - not just treat the symptoms.
Key Takeaways
- Allergic asthma affects 60% of adults and 80% of children with asthma - it’s the most common form.
- Triggers are specific: pollen, dust mites, pet dander, mold. Know yours.
- Avoidance works: HEPA filters, humidity control, washing bedding hot, and showering after being outside make a measurable difference.
- Immunotherapy is the only treatment that changes your immune system’s response - and it can reduce medication use by 40%.
- Not all ‘allergic asthma’ is truly allergic. Get biomarker tests (eosinophils, FeNO) to confirm before spending on expensive biologics or immunotherapy.
- New tech like AI predictors and nasal sensors are making management easier than ever.



Steve Sullivan
December 8, 2025 AT 16:20Richard Eite
December 9, 2025 AT 05:25Katherine Chan
December 11, 2025 AT 02:10Philippa Barraclough
December 11, 2025 AT 19:33Olivia Portier
December 12, 2025 AT 19:12Ajit Kumar Singh
December 13, 2025 AT 18:32Simran Chettiar
December 15, 2025 AT 01:43Andrea Petrov
December 16, 2025 AT 01:35Tim Tinh
December 17, 2025 AT 01:46Tiffany Sowby
December 18, 2025 AT 10:02Delaine Kiara
December 19, 2025 AT 22:12Anna Roh
December 20, 2025 AT 17:17