Many older adults take medications every day to manage pain, allergies, overactive bladder, or depression. But what if some of these everyday pills are quietly damaging their memory? The answer isn’t theoretical-it’s backed by years of brain scans, long-term studies, and real-life stories from families watching their loved ones change. This isn’t about rare side effects. It’s about a hidden pattern: the cumulative power of anticholinergic drugs, and how they’re quietly increasing the risk of cognitive decline in older adults.
What Exactly Is Anticholinergic Burden?
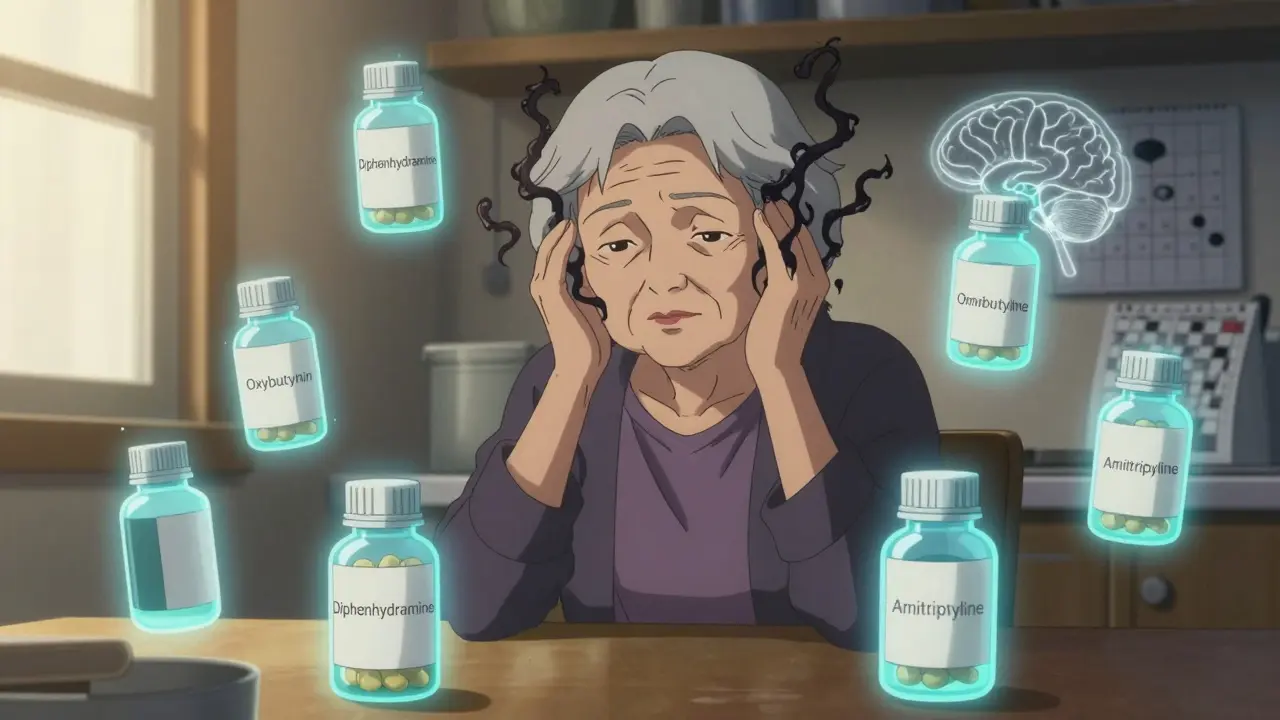
Anticholinergic burden (ACB) is the total effect of all medications that block acetylcholine, a key brain chemical for memory, focus, and learning. It’s not about one drug-it’s about the sum of all the pills you take. A person might be on a low-dose antihistamine for allergies, a tricyclic antidepressant for nerve pain, and a bladder medication for urgency. Individually, each might seem harmless. Together, they add up. The most widely used tool to measure this is the Anticholinergic Cognitive Burden (ACB) scale. It ranks drugs into three levels:- Level 1: Mild effect (like some antihistamines)
- Level 2: Moderate effect (like certain antidepressants)
- Level 3: Strong effect (like oxybutynin or diphenhydramine)
How These Drugs Actually Affect the Brain
Acetylcholine isn’t just a chemical-it’s the brain’s communication wire for memory and attention. The M1 muscarinic receptor, where anticholinergics bind, is packed in the hippocampus and frontal cortex. These are the exact areas that shrink in Alzheimer’s disease. Brain imaging studies show something startling. In a 2016 JAMA Neurology study, older adults taking just one or two strong anticholinergic drugs had 4% less glucose metabolism in the temporal lobe-the same region that goes quiet in early Alzheimer’s. Even people with no memory complaints showed this drop. That’s not normal aging. That’s drug-induced brain slowdown. MRI scans from the Indiana Memory and Aging Study found that long-term users of anticholinergics lost brain volume 0.24% faster per year than non-users. That might sound small, but over five years, that’s nearly 1.2% more brain shrinkage. That’s the equivalent of accelerating aging by a decade.Cognitive Domains Most at Risk
Not all memory suffers equally. Research from the ASPREE trial-tracking over 19,000 adults over 70-showed which areas are hit hardest:- Executive function: Planning, organizing, switching tasks. Each 1-point increase in ACB score led to a 0.15-point decline per year on word association tests.
- Episodic memory: Remembering recent events or conversations. Each ACB point meant a 0.08-point drop per year on recall tests.
- Processing speed: How fast you react or solve simple problems. Here, the effect was barely noticeable.

The Dose-Response Reality
The longer you take these drugs, the worse it gets. A landmark 2015 study from the University of Washington found that people who took strong anticholinergics for three years or more had a 54% higher risk of dementia than those who took them for less than three months. The risk didn’t plateau-it climbed steadily with time. And it’s not just about pills you’re prescribed. Many older adults self-medicate. A 2021 survey by the National Council on Aging found that 63% of seniors were never told their medication could hurt their memory. One woman in Sydney told her doctor she was having trouble remembering names. She didn’t mention she took Benadryl every night for sleep. Her doctor didn’t connect the dots.Real People, Real Changes
The most powerful evidence isn’t in journals-it’s in lived experience. On AgingCare.com, dozens of caregivers describe the same pattern:“My mom was confused all the time. She’d forget meals, get lost walking to the mailbox. We thought it was early dementia. Then her pharmacist flagged her meds-oxybutynin, amitriptyline, diphenhydramine. We stopped them. Within two weeks, she was herself again. Her doctor said it was ‘just aging.’ But she was fine before the meds.”The FDA recorded over 1,200 cognitive adverse events in seniors between 2018 and 2022. The top three? Confusion, memory loss, and delirium. All reversible-if you catch them early.
What’s Being Done-and What’s Not
The American Geriatrics Society’s 2023 Beers Criteria explicitly warns against using strong anticholinergics in older adults. The European Medicines Agency banned dimenhydrinate in dementia patients. The FDA now requires warning labels on all anticholinergic drugs. But here’s the gap: only 38.7% of nursing home residents with high anticholinergic scores had their meds reviewed within three months of being flagged. Primary care doctors say they need 23 minutes per patient to do a full medication review. Most appointments are 10 minutes. Pharmaceutical companies are responding. Johnson & Johnson pulled long-acting oxybutynin in 2021. Pfizer pushed solifenacin (VESIcare), which doesn’t cross the blood-brain barrier as easily. Newer bladder drugs are safer. But many older prescriptions are still being refilled automatically.What You Can Do Today
If you or someone you care about is over 65 and on multiple medications:- Make a full list of every pill, patch, cream, and OTC product-including sleep aids, allergy pills, and stomach remedies.
- Check the ACB score using the American Geriatrics Society’s free ACB Calculator app (launched in 2024). It’s simple: enter the drug names, and it tells you the total burden.
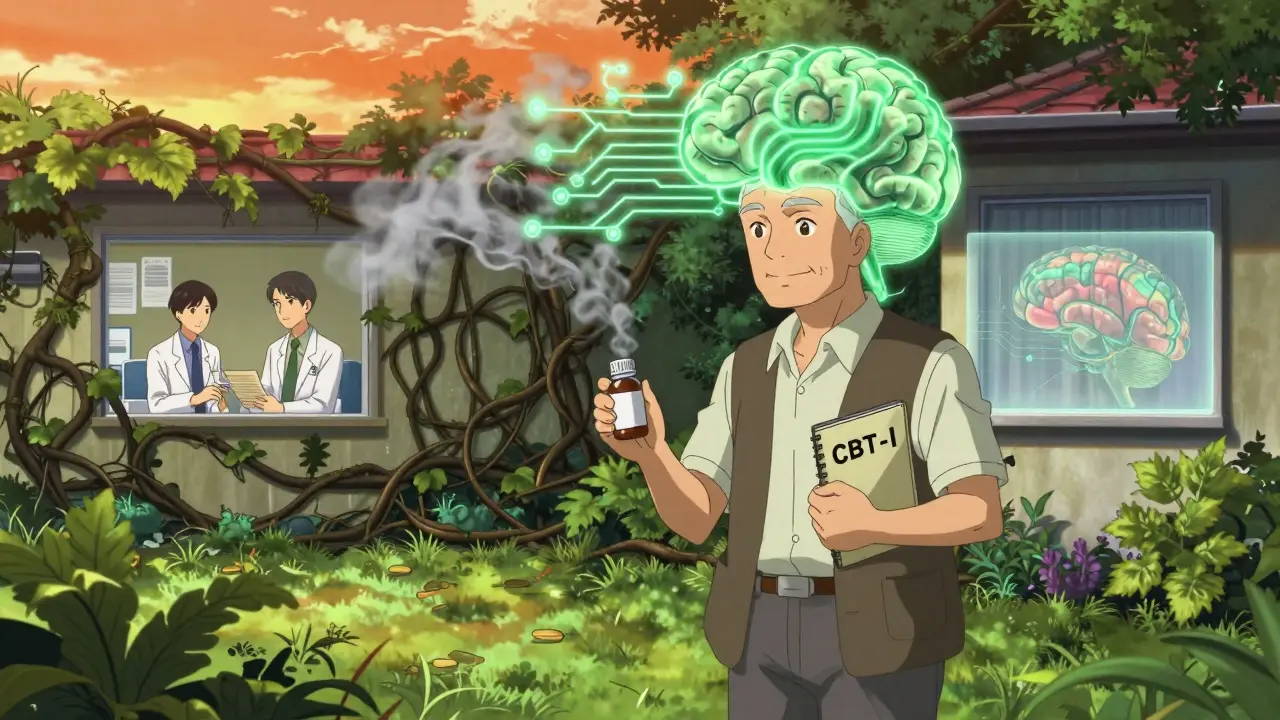
- Ask your doctor: “Is there a non-anticholinergic alternative?” For bladder issues, mirabegron (Myrbetriq) is now preferred over oxybutynin. For depression, SSRIs like sertraline have almost no anticholinergic effect. For sleep, melatonin or cognitive behavioral therapy beats diphenhydramine.
- Don’t stop cold turkey. Some drugs need to be tapered. Work with your doctor or pharmacist. The DICE trial showed cognitive improvements took 12 weeks-but they happened.
Why This Matters More Than Ever
By 2030, one in five Australians will be over 65. Dementia rates are rising. But research now suggests anticholinergic burden could be responsible for 10-15% of dementia cases in older adults. That’s not inevitable. It’s preventable. This isn’t about fear. It’s about awareness. Many of these drugs were prescribed decades ago and never re-evaluated. The brain changes they cause are real, measurable, and often reversible-if you act. The best part? You don’t need a specialist. You just need to ask the right questions. And you don’t have to wait for a diagnosis to start protecting memory. Start today-with a list of pills, a phone call to your pharmacist, and the courage to say, “Is this really necessary?”Can anticholinergic drugs cause dementia?
They don’t directly cause dementia, but long-term use significantly increases the risk. Studies show people taking high anticholinergic burden medications for three or more years have a 54% higher chance of developing dementia compared to those who take them briefly. The drugs accelerate brain changes linked to Alzheimer’s, including reduced metabolism and faster brain shrinkage. This is one of the few modifiable risk factors for cognitive decline.
What are the most common anticholinergic medications for seniors?
The top three drug classes are: 1) First-generation antihistamines like diphenhydramine (Benadryl), often used for sleep or allergies; 2) Antimuscarinics for overactive bladder like oxybutynin and tolterodine; and 3) Tricyclic antidepressants like amitriptyline and nortriptyline, used for pain or depression. These are all Level 3 on the ACB scale, meaning they have strong effects on the brain.
Can memory improve after stopping these drugs?
Yes, in many cases. The DICE trial showed that after 12 weeks of reducing or stopping anticholinergic drugs, older adults improved their Mini-Mental State Exam (MMSE) scores by an average of 0.82 points. Caregivers report noticeable improvements in confusion and memory within two to four weeks. The brain has remarkable plasticity-once the drug’s effect is lifted, cognitive function often rebounds, especially if there’s no underlying neurodegenerative disease.
Are over-the-counter sleep aids safe for seniors?
Most are not. Common OTC sleep aids like Unisom, Sominex, and NyQuil contain diphenhydramine or doxylamine-both strong anticholinergics. Even one pill a night adds up over time. For seniors, safer options include melatonin (in low doses), cognitive behavioral therapy for insomnia (CBT-I), or addressing underlying causes like sleep apnea. Never assume OTC means safe for older adults.
How can I check my anticholinergic burden?
Use the free ACB Calculator app from the American Geriatrics Society. It’s designed for patients and caregivers. Just enter the names of all your medications-including supplements and OTC drugs-and it calculates your total ACB score. You can also ask your pharmacist for a medication review. Many pharmacies now offer this service at no cost. Write down your list before your appointment and bring it with you.
What are safer alternatives to anticholinergic drugs?
For overactive bladder: mirabegron (Myrbetriq) or pelvic floor therapy. For depression: SSRIs like sertraline or citalopram. For allergies: non-sedating antihistamines like loratadine or fexofenadine. For insomnia: melatonin, CBT-I, or improving sleep hygiene. For chronic pain: physical therapy, acetaminophen, or non-anticholinergic nerve pain meds like gabapentin. Always ask your doctor: “Is there a non-anticholinergic option?”



John O'Brien
January 27, 2026 AT 02:59This is wild. My grandma was on Benadryl every night for years and we thought she was just getting forgetful. Turns out she was just drugged up. We pulled her off it and she started remembering our names again. No joke. Pharmacies are literally selling brain rot as sleep aids.
Paul Taylor
January 27, 2026 AT 17:55Look I get it people are scared of meds but this is just another scare tactic dressed up as science. Everyone’s got a different brain chemistry. Some people take these drugs for decades and stay sharp. Others get hit by a bus at 70 and suddenly it’s the meds. Correlation isn’t causation and the brain shrinks with age anyway. Stop blaming pills for normal aging. The real issue is we’ve turned every minor inconvenience into a medical emergency.
Desaundrea Morton-Pusey
January 27, 2026 AT 19:33Of course the FDA didn’t do anything until it was too late. Big Pharma’s been pushing these drugs since the 80s because they’re cheap and profitable. They don’t care if you forget your grandkids’ birthdays as long as you keep buying the next bottle. This is why I don’t trust any doctor who takes a free lunch from a rep.
Murphy Game
January 29, 2026 AT 12:07Did you know the WHO quietly classified anticholinergics as neurotoxins in 2019 but buried the report? And the CDC? They’ve been deleting studies on this since 2017. Why? Because Medicare spends $200 billion a year on these prescriptions. They’d rather watch you turn into a zombie than admit the system’s broken. Wake up.
Kegan Powell
January 30, 2026 AT 06:09Bro this is the most important thing I’ve read all year 🙏 I’m 68 and on 3 of these meds. Just pulled up the ACB app and my score was 7. I’m calling my pharmacist tomorrow. If we can reverse this with a phone call and a list of pills? That’s not just smart. That’s freedom. The brain is not a fixed thing. It’s alive. And we’ve been poisoning it with convenience. Time to choose differently.
April Williams
January 30, 2026 AT 07:40How is this even legal? People are dying from this and no one’s going to jail? My uncle’s dementia started after his doctor gave him amitriptyline for back pain. He was fine before. Now he doesn’t know who I am. Where’s the accountability? This isn’t negligence. This is criminal. Someone needs to be prosecuted.
Harry Henderson
February 1, 2026 AT 03:34STOP SCROLLING. START LISTING. Right now. Open your medicine cabinet. Write down every pill. Every OTC thing you take. Every cream. Every nightcap. Then go to the ACB app. Don’t wait. Don’t rationalize. Do it. Your future self will thank you. This isn’t a suggestion. It’s an emergency.
suhail ahmed
February 2, 2026 AT 23:23Man this hits different. In India we call these meds 'sleepy pills' and grandmas take them like candy. No one tells them about the brain fog. My aunt stopped her oxybutynin and suddenly she was singing old Bollywood songs again. She hadn’t done that in years. The body remembers. The brain remembers. Just remove the poison and watch the light come back. Simple. But nobody wants to believe it’s that simple.
Candice Hartley
February 4, 2026 AT 05:59I’m 72. Took diphenhydramine for 10 years. Stopped. Two weeks later I could follow a movie plot again. 🙌
astrid cook
February 4, 2026 AT 21:21Of course you’re telling people to stop their meds. You didn’t read the full study. The DICE trial only included people with no prior cognitive impairment. What about those already on the edge? You’re just giving people false hope. This isn’t a fix. It’s a gamble. And someone’s going to get hurt.
Andrew Clausen
February 5, 2026 AT 21:05The article incorrectly conflates correlation with causation. The cited JAMA Neurology study adjusted for baseline cognition but did not control for polypharmacy or comorbid conditions. The 54% increased dementia risk was only significant in the highest quintile of exposure, not the general population. Also, 'Level 3' is not a standardized FDA classification. The ACB scale is a research tool, not a clinical diagnostic. This post is dangerously oversimplified.