Paget's Disease Bone Density Assessment Tool
Analysis Results
Bone Status:
Disease Activity:
Treatment Recommendation:
Fracture Risk:
Next Steps:
About This Tool
This tool interprets bone density test results for Paget's disease patients. It combines T-score values with alkaline phosphatase levels to provide insights into bone health status, disease activity, and treatment recommendations. Remember, this is for educational purposes only and should not replace professional medical advice.
Key Takeaways
- Bone density testing identifies abnormal bone remodeling early in Paget’s disease.
- DXA scan results guide bisphosphonate dosing and monitor treatment response.
- Combining T‑score data with serum alkaline phosphatase gives a fuller picture of disease activity.
- Regular testing reduces fracture risk by informing timely lifestyle and medication adjustments.
- Understanding test limitations prevents misinterpretation and unnecessary anxiety.
When dealing with bone density testing a non‑invasive scan that measures the mineral content of bone, helping clinicians evaluate strength and fracture risk in patients who have Paget’s disease a chronic disorder that disrupts normal bone remodeling, causing bone enlargement and structural weakness, the test becomes more than a routine check‑up-it’s a decision‑making tool. Below we break down why this test matters, how it works, and how to turn numbers into real‑world treatment steps.
1. How Bone Density Testing Works in Paget’s Disease
The most common method is the dual‑energy X‑ray absorptiometry (DXA) scan. DXA sends two low‑dose X‑ray beams through the bone, usually at the lumbar spine and hip, and calculates the bone mineral density (BMD) from the differential absorption.
DXA scan provides a precise BMD measurement expressed as a T‑score, which compares the patient’s bone density to a healthy 30‑year‑old reference. The test takes about 10‑15 minutes, involves no anesthesia, and delivers radiation comparable to a day’s natural background exposure.
2. Interpreting the Numbers: T‑Score, Z‑Score, and What They Mean for Paget’s
The output includes two scores:
- T‑score: compares your BMD to a young adult reference. A T‑score above -1 is considered normal, between -1 and -2.5 signals osteopenia, and -2.5 or lower indicates osteoporosis.
- Z‑score: compares your BMD to age‑matched peers, useful for secondary conditions like Paget’s where age‑related bone loss may coexist.
In Paget’s disease, the affected region can show an inflated BMD due to disorganized new bone formation, while neighboring sites may be osteoporotic. That’s why clinicians look at both the local and contralateral measurements.
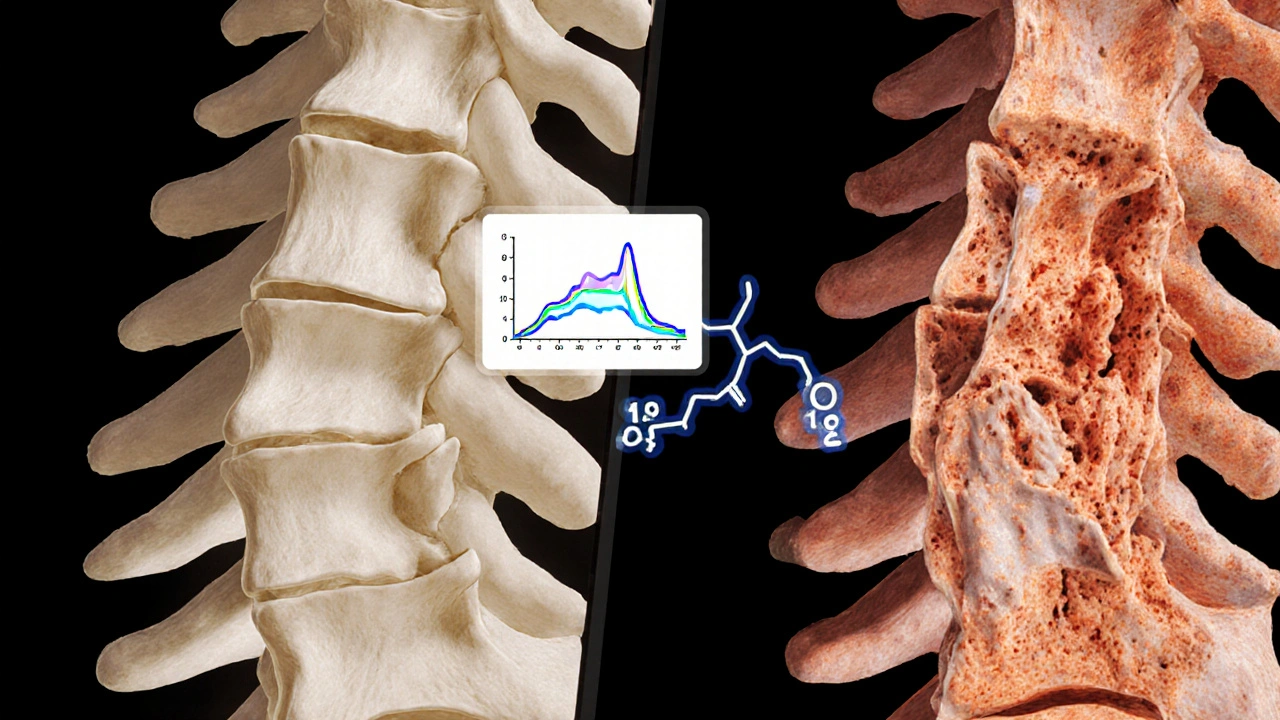
3. Linking Test Results to Disease Activity Markers
Bone density alone doesn’t capture the metabolic frenzy of Paget’s. Serum alkaline phosphatase is an enzyme released by active bone‑forming cells; elevated levels signal high disease activity are a hallmark. Combining a high alkaline phosphatase reading with a normal or high T‑score in the same site suggests active remodeling, whereas a low T‑score with normal enzyme levels may point to underlying osteoporosis unrelated to Paget’s.
Using the WHO criteria for osteoporotic classification based on T‑score thresholds alongside enzyme data gives a more nuanced risk profile.
4. How Test Outcomes Shape Treatment Decisions
Bisphosphonate therapy the first‑line medication for slowing bone turnover in Paget’s disease dosage and duration are often calibrated to the baseline BMD and alkaline phosphatase levels. For example:
- If the DXA shows osteopenia (T‑score -1 to -2.5) and alkaline phosphatase is modestly elevated, a standard oral bisphosphonate course (e.g., alendronate 40mg weekly) is typical.
- If the site’s BMD is high but the enzyme spikes >2× upper‑limit‑normal, an intensive intravenous bisphosphonate (zoledronic acid 5mg) is preferred to quickly suppress turnover.
- When osteoporosis (T‑score ≤ -2.5) coexists, clinicians may combine bisphosphonate with calcium and vitaminD supplementation to support overall bone health.
Monitoring BMD every 12‑18months after treatment start helps verify that the medication is stabilizing bone density and that the disease isn’t progressing silently.
5. Lifestyle and Nutritional Support Complementing the Scan
Even with optimal medication, patients need adequate calcium a mineral essential for bone mineralization; recommended intake for adults is 1,000mg/day (1,200mg for women over 50) and vitaminD facilitates calcium absorption; levels above 30ng/mL are associated with reduced fracture risk. Weight‑bearing exercise (e.g., walking, resistance training) further stimulates bone strength without overloading the affected sites.

6. Pitfalls: When Bone Density Testing Can Mislead
Because Paget’s can produce overly dense but structurally weak bone, a single DXA reading may mask fracture risk. Common misinterpretations include:
- Assuming a high T‑score means low fracture risk, ignoring the irregular microarchitecture.
- Failing to scan the contralateral side, which may reveal true osteoporosis.
- Relying solely on DXA without checking alkaline phosphatase trends.
To avoid these traps, clinicians should combine imaging (DXA + radiographs) with biochemical markers and clinical assessment (pain, deformity, functional limitation).
7. Practical Checklist for Patients and Providers
| Step | What to Do | Why It Matters |
|---|---|---|
| 1 | Order a DXA scan of lumbar spine, hip, and affected bone site. | Establish baseline BMD and identify mixed density patterns. |
| 2 | Measure serum alkaline phosphatase. | Quantify disease activity to pair with imaging. |
| 3 | Calculate T‑score and Z‑score; compare to WHO thresholds. | Classify bone health (normal, osteopenia, osteoporosis). |
| 4 | Review calcium and vitaminD intake; supplement if needed. | Support mineralization and improve treatment response. |
| 5 | Choose bisphosphonate regimen based on BMD + enzyme level. | Target therapy to suppress excessive turnover. |
| 6 | Schedule follow‑up DXA in 12‑18months. | Detect changes early and adjust therapy. |
8. Frequently Asked Questions
Frequently Asked Questions
How often should someone with Paget’s disease get a bone density test?
After the initial diagnosis, a DXA scan is recommended every 12‑18months, especially when a bisphosphonate has been started or altered. If disease activity is stable and BMD is normal, extending the interval to 2‑3years may be safe.
Can a high T‑score ever indicate a problem in Paget’s disease?
Yes. Paget’s can produce dense but architecturally abnormal bone. A high T‑score in the affected segment may mask a fracture‑prone structure, so clinicians also look at alkaline phosphatase and compare to the opposite side.
Is DXA safe for people with metal implants?
DXA uses low‑energy X‑rays, and most metal implants cause only minimal artifact. If the implant is near the scanned region, the technician may adjust the scan site or use a different modality like quantitative CT.
What lifestyle changes boost the benefit of bone density testing?
Adequate calcium (1,000‑1,200mg daily) and vitaminD (800‑1,000IU), regular weight‑bearing exercise, and avoiding smoking or excess alcohol all improve bone health and make test results more predictive of real‑world outcomes.
Can bone density testing replace other imaging for Paget’s?
No. DXA quantifies mineral density, but plain radiographs or MRI are needed to assess bone deformation, cortical thickening, and to guide surgical planning when needed.
In a nutshell, bone density testing isn’t just a number‑checking exercise for Paget’s disease-it’s the compass that steers medication, lifestyle tweaks, and monitoring schedules. By pairing precise DXA data with biochemical markers and a proactive care plan, patients can keep the disease in check and drastically lower their chance of painful fractures.



Richard Gerhart
October 5, 2025 AT 17:50Hey folks, just a heads‑up that regular bone density scans are a game‑changer for anyone dealing with Paget’s disease. Even if you feel fine, the DEXA results can flag hidden hotspots before they turn into painful fractures. I’d say aim for a baseline test now, then follow up every 1‑2 years or sooner if your alkaline phosphatase spikes. Talk to your endocrinologist about the best schedule for you – they’ll tailor it to your age and which bone sites are affected. And remember, staying active and getting enough calcium and vitamin D can keep those numbers in the green. Stay on top of it, dont wait till the pain tells you something’s wrong!
Kim M
October 5, 2025 AT 23:33Yo, this whole bone density gizmo looks legit but have you ever wondered who's really profiting from it? 🤔 The pharma giants push these tests so they can sell you pricey bisphosphonates later. 🌐 Stay skeptical and ask for raw data before you get swept into the treatment loop. 😊
Martin Gilmore
October 6, 2025 AT 07:53THIS IS NOT A DRILL!!! The importance of BONE DENSITY TESTING IN PAGET'S IS OFF THE CHARTS!!! If you skip it, you’re practically signing up for catastrophic fractures!!! The T‑SCORE AND ALK PHOS LEVELS ARE YOUR LIFELINE-DO NOT IGNORE!!!
jana caylor
October 6, 2025 AT 12:03While I appreciate the enthusiasm, let’s keep the tone measured. Bone density testing is indeed valuable, but alarmist language can cause unnecessary worry. It’s best to discuss results calmly with a healthcare professional.
Vijendra Malhotra
October 6, 2025 AT 16:13Friends, in many Indian families we treat bone health as a community responsibility. Regular scans help us plan diet rich in calcium‑laden foods like paneer and almonds. I urge you to schedule your DEXA early, especially if you have a family history of Paget’s. Aggressive monitoring can prevent costly complications later. Stay proactive and share your schedule with your doctor – they’ll appreciate your diligence.
Hannah Gorman
October 7, 2025 AT 03:20When it comes to managing Paget’s disease, a comprehensive approach is absolutely essential, and bone density testing sits at the very heart of that strategy.
First and foremost, the DEXA scan provides an objective measurement of mineral content, which is something that no subjective symptom reporting can replace.
Moreover, the correlation between elevated alkaline phosphatase and accelerated bone turnover makes it imperative to pair biochemical markers with imaging for a full picture.
In my experience, patients who delay their baseline scan often find themselves confronting unexpected fractures that could have been mitigated with earlier intervention.
The literature consistently shows that early detection allows clinicians to initiate bisphosphonate therapy in a timely manner, thereby reducing both pain and deformity.
It is also worth noting that the specific anatomical site assessed-whether lumbar spine, hip, or another region-can influence treatment decisions, given the variable involvement patterns seen in Paget’s.
Age is another crucial factor; younger adults may tolerate aggressive therapy better than seniors, who are at higher risk for side effects.
Patients should also be educated about the significance of T‑scores: a reading above –1 is generally reassuring, whereas values below –2.5 signal osteoporotic risk that necessitates immediate attention.
Even those with T‑scores in the osteopenic range should not be complacent, as Paget’s can accelerate bone loss beyond typical expectations.
Additionally, periodic monitoring of alkaline phosphatase trends can flag disease flare‑ups before structural damage becomes evident on imaging.
I have observed that clinicians who rely solely on symptomatology often miss subclinical disease activity, leading to suboptimal outcomes.
From a health‑economics perspective, routine testing is cost‑effective, as it offsets the expenses associated with fracture management and long‑term disability.
It is also prudent to involve a multidisciplinary team-rheumatologists, endocrinologists, and physical therapists-to address the multifaceted needs of Paget’s patients.
Patients who engage actively in their care, adhering to scheduled scans and medication regimens, typically report higher quality of life scores.
Finally, while this tool offers valuable educational insight, it should never replace personalized medical advice from a qualified practitioner.
Keli Richards
October 7, 2025 AT 17:13I agree with your thorough overview and would add that patient education on lifestyle modifications can further enhance outcomes. Regular exercise, balanced nutrition, and fall‑prevention strategies complement the diagnostic data you highlighted.
Tom Druyts
October 8, 2025 AT 07:06Yo, smash that bone density test and take control of your Paget’s journey! Every scan is a power‑up toward stronger bones-let’s do this! 💪
Zuber Zuberkhan
October 8, 2025 AT 21:00Absolutely, Tom! Consistency with testing builds confidence and keeps us ahead of any flare‑ups. Let’s keep the momentum and encourage others to stay on schedule.
Tara Newen
October 9, 2025 AT 10:53Frankly, most people underestimate how critical serial DEXA measurements are; the data you ignore today becomes a liability tomorrow. Ignorance in this arena equates to reckless health management.
Amanda Devik
October 10, 2025 AT 00:46Listen up-your osteopenia risk isn’t a vague concept, it’s a quantifiable metric that can be mitigated with targeted anti‑resorptive therapy and biomechanical loading protocols. Embrace the data, trust the algorithm, and let’s turn those numbers into a victory.
Mr. Zadé Moore
October 10, 2025 AT 14:40The tool is a half‑baked gimmick.