Every year, thousands of people die not from taking one dangerous drug, but from mixing two or more that seem harmless on their own. It’s not always heroin or cocaine alone that kills-it’s when those drugs meet alcohol, Xanax, or even a common painkiller. The truth is, many of the deadliest drug combinations aren’t street drugs at all. They’re prescriptions you got from a doctor, mixed with a glass of wine or a few beers after work. These aren’t myths. They’re documented, preventable tragedies.
Why Mixing Drugs Is More Dangerous Than You Think
Drugs don’t just add up when you mix them-they multiply. Take opioids and alcohol. Individually, both slow your breathing. Together, they can shut it down completely. Research shows this combo increases the risk of respiratory failure by 4.5 times compared to either drug alone. It doesn’t matter if you’re taking a low dose of oxycodone after dental surgery or a prescription for chronic pain. Two drinks can be enough to push you over the edge.
This isn’t theoretical. In 2021, nearly half of all cocaine overdose deaths in the U.S. involved heroin. That’s the infamous ‘speedball.’ People think the stimulant (cocaine) cancels out the depressant (heroin), but that’s a deadly lie. Instead, your heart races, your blood pressure spikes, and your lungs struggle to keep up. The result? Heart attack, stroke, or sudden respiratory arrest. Celebrities like River Phoenix and John Belushi didn’t die from one drug-they died from the collision of two.
The Most Deadly Combinations You Need to Know
- Opioids + Benzodiazepines: This is the most common lethal mix in modern overdose deaths. In 2020, over 30% of opioid-related deaths also involved drugs like Xanax, Valium, or Ativan. Both calm your nervous system. Together, they can stop your breathing while you’re asleep. The CDC says this combo is behind a growing number of accidental deaths, even among people taking their prescriptions exactly as directed.
- Alcohol + Opioids: Alcohol doesn’t just make painkillers stronger-it makes them deadlier. The liver can’t process both at once. Side effects include extreme drowsiness, confusion, vomiting, and loss of consciousness. Even one drink can turn a safe dose into a fatal one.
- Alcohol + Cocaine: This mix creates a toxic chemical called cocaethylene in your liver. It lasts longer than cocaine, gives you a longer high, and is 25% more likely to kill you. It also damages your liver, increases your heart rate to dangerous levels (often over 140 bpm), and raises your risk of seizures and heart attack. People who drink and do cocaine often don’t realize how much they’ve taken because the alcohol masks the high.
- Alcohol + Antidepressants (like Effexor or Cymbalta): You might think it’s fine to have a glass of wine while on antidepressants. It’s not. Alcohol increases the risk of liver damage by up to 40% with drugs like Cymbalta. With venlafaxine, it lowers your tolerance for alcohol so much that a normal night out can lead to fatal poisoning. Mood stabilizers don’t protect you-they make you more vulnerable.
- Buprenorphine + Alcohol: Buprenorphine is used to treat opioid addiction. But if you drink while taking it, your blood pressure can crash, your breathing can slow to under 10 breaths per minute, and you can slip into a coma. The SA Health Department warns: “The more alcohol in your body, the less heroin you need to die.” The same applies to buprenorphine.
- Stimulants + Stimulants (Cocaine + Methamphetamine): Mixing stimulants doesn’t give you more energy-it pushes your heart and brain past their limits. This combo increases the risk of psychosis by 35%, triggers panic attacks in 60-70% of users, and can cause seizures or sudden cardiac arrest. People often take more because they don’t feel the effects right away, not realizing they’ve already crossed into danger.
What Happens in Your Body When Drugs Collide
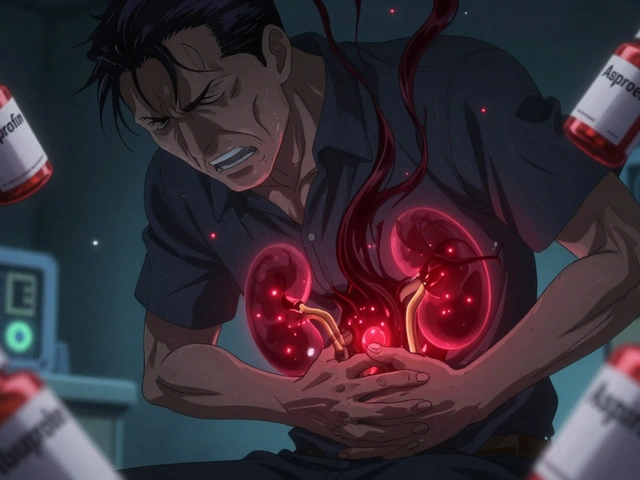
Your body doesn’t see drugs as ‘prescription’ or ‘illicit.’ It sees chemicals-and it tries to process them the same way. When two drugs compete for the same liver enzymes, they back up like traffic. That’s why alcohol and acetaminophen (found in Vicodin and Percocet) can destroy your liver. One drink might be fine. Two with your painkiller? That’s a recipe for acute liver failure.
Other combinations overload your nervous system. Benzodiazepines and opioids both bind to GABA receptors in your brain, which control relaxation and breathing. When both are present, your brain stops signaling your lungs to breathe. You don’t feel it coming. You just stop. No struggle. No warning. That’s why so many overdoses are found in bed-people never woke up.
Then there’s cocaethylene, the hidden killer in alcohol-cocaine mixes. It’s not just more toxic-it’s harder for your body to clear. It stays in your system longer, meaning the danger doesn’t end when the high does. Chronic users develop liver scarring, weakened immunity, and a higher chance of sudden death even days after using.

Real Stories, Real Consequences
Reddit threads from r/StopDrinking and r/opiates are full of near-death accounts. One user took oxycodone after a tooth extraction. He had two beers. He stopped breathing. His roommate found him blue, called 911, and administered naloxone just in time. Another took Xanax and vodka to sleep. He woke up 10 hours later with no memory of the night, covered in vomit, and terrified he’d died without knowing it.
These aren’t rare cases. They’re typical. A 2023 study found that 78.3% of fatal opioid overdoses involved another substance. Most often: benzodiazepines, cocaine, or alcohol. And the numbers are rising. Between 2019 and 2022, concurrent use of opioids and benzodiazepines increased by 15% in the U.S. That’s not progress. That’s a warning.
How to Protect Yourself and Others
Here’s what actually works:
- Ask your doctor or pharmacist about every medication you take-including supplements and OTC pain relievers. Don’t assume it’s safe. Many people don’t know that NyQuil contains alcohol and acetaminophen, which can be deadly with opioids.
- Read the label. If it says ‘avoid alcohol’ or ‘may cause drowsiness,’ take it seriously. That’s not a suggestion. It’s a life-or-death warning.
- Don’t mix street drugs with anything. Fentanyl is in 6 out of 10 counterfeit pills. You think you’re taking oxycodone. You’re not. You’re taking something that could kill you with one pill-no alcohol needed.
- Carry naloxone. If you or someone you know uses opioids, even occasionally, keep naloxone on hand. It won’t reverse alcohol or benzodiazepine overdoses, but it can save a life if opioids are involved. Many community centers in Sydney and across Australia now give it out for free.
- Know the signs of overdose: Slow or stopped breathing, blue lips or fingernails, unresponsiveness, gurgling sounds, limp body. If you see these, call emergency services immediately. Don’t wait. Don’t try to ‘sleep it off.’

What’s Changing to Prevent These Deaths
Health systems are catching up. Since 2019, Medicare Part D plans in the U.S. have been required to flag opioid-benzodiazepine prescriptions. The result? An 18% drop in dangerous co-prescribing. Pharmacies now use automated alerts. Electronic health records are starting to warn doctors before they write a prescription that could kill.
AI-powered drug interaction checkers are becoming standard. Tools like WebMD’s checker and Medscape’s database are now used in clinics across Australia and the U.S. They’re not perfect-but they’re better than guessing.
Public awareness campaigns are also making a difference. SAMHSA’s 2023 initiative led to a 27% increase in calls to poison control centers about drug mixing. That’s not a bad thing. It means people are asking questions before it’s too late.
Bottom Line: It’s Not About Willpower
People don’t die from drug mixing because they’re reckless. They die because they didn’t know. They thought one drink wouldn’t hurt. They trusted their doctor’s prescription. They didn’t realize their painkiller contained alcohol. They didn’t know fentanyl was in the pill they bought online.
Safety isn’t about being perfect. It’s about being informed. If you’re on any medication-especially for pain, anxiety, or depression-ask: ‘Could this kill me if I drink, smoke, or take something else?’ If you’re helping someone struggling, don’t judge. Ask them what they’re taking. Offer naloxone. Share this list.
One conversation could save a life. Not tomorrow. Today.
Can I have one drink while taking painkillers?
No. Even one standard drink can double your risk of respiratory depression when mixed with opioids like oxycodone or hydrocodone. Your liver can’t process both safely. What feels like a small amount can be enough to stop your breathing. Always assume alcohol and painkillers don’t mix.
Is it safe to take Xanax and drink alcohol if I space them out?
No. Benzodiazepines stay in your system for hours-even days. Spacing them out doesn’t help. The combined effect on your brain and breathing is still dangerous. Many people who overdose on this combo didn’t take them at the same time-they just took them hours apart. The drugs still interact inside your body.
What should I do if someone overdoses on a drug mix?
Call emergency services immediately. If you have naloxone and opioids are involved, administer it. Even if you’re unsure, give it-it won’t harm someone who doesn’t need it. Keep the person awake and breathing. If they’re unconscious, place them on their side to prevent choking. Do not leave them alone. Do not try to make them vomit or give them coffee. Wait for paramedics.
Are over-the-counter meds safe to mix with alcohol?
Not always. Many OTC pain relievers like Tylenol (acetaminophen) can cause severe liver damage when mixed with alcohol. Cold and flu medicines often contain alcohol or sedating antihistamines. Always check the label for warnings. If it says ‘avoid alcohol,’ it’s not a suggestion-it’s a warning.
Why are fentanyl-laced pills so dangerous with other drugs?
Fentanyl is 50-100 times stronger than morphine. A pill you think is oxycodone might contain a lethal dose of fentanyl. Add alcohol, benzodiazepines, or stimulants, and your body has no chance. There’s no safe dose when fentanyl is involved. Even if you’ve used the same drug before, this batch could be deadly. Testing strips can help-but they’re not foolproof. The safest choice is to avoid unknown pills entirely.
Can I use cannabis with prescription drugs?
Cannabis can interact with many medications, especially those that affect the liver or central nervous system. It can increase drowsiness with opioids and benzodiazepines, and may worsen side effects of antidepressants. There’s limited research, but the risk is real. Always talk to your doctor before mixing cannabis with any prescription.
If you’re taking medication, talk to your pharmacist. If you’re helping someone, share this information. No one should die because they didn’t know.




Tom Shepherd
November 27, 2025 AT 14:29Just had my dentist prescribe oxycodone and I was gonna have a beer after dinner. Read this and put the bottle back in the fridge. Scary how something so normal can kill you.
Gayle Jenkins
November 29, 2025 AT 08:09This is the kind of post that should be mandatory reading in every high school health class. Not just for drug users-for everyone. I work in ER and we see this every damn weekend. People think they’re being smart by spacing out their meds or drinking ‘just one.’ No. Your body doesn’t care about your schedule. It just dies quietly.
My cousin took Xanax and had two glasses of wine. Thought she was just sleepy. Woke up in the ICU with no memory of it. She’s fine now. But she won’t ever touch that combo again. Don’t wait for your near-death experience to learn this.
Gaurav Sharma
November 30, 2025 AT 02:13It is imperative to underscore that the pharmacokinetic interactions described herein are not merely anecdotal but are empirically validated through peer-reviewed toxicological studies. The confluence of GABAergic depressants with opioid receptor agonists constitutes a synergistic respiratory depressant cascade, the clinical manifestation of which is invariably fatal absent immediate intervention.
Kaleigh Scroger
December 1, 2025 AT 12:28People don’t realize how long these drugs stick around. I used to think if I took my Xanax at night and had a glass of wine at dinner the next day it was fine. Wrong. Benzodiazepines have half-lives of up to 50 hours. That means even after two days there’s still enough in your system to team up with alcohol and shut your lungs down. I learned this the hard way after my mom went to the hospital. She didn’t even know she was mixing them. She thought she was being careful. That’s the worst part-no one thinks they’re the one who’s gonna die.
And don’t get me started on OTC meds. NyQuil has alcohol. DayQuil has dextromethorphan which can be deadly with antidepressants. Tylenol is acetaminophen. One drink with that after a long day? Liver failure. No drama. No warning. Just gone. I’ve seen it. I’ve held people’s hands while they waited for a transplant that never came. This isn’t scare tactics. This is reality.
And if you’re on buprenorphine? Don’t even think about it. That stuff is designed to keep you alive but alcohol turns it into a suicide pill. SA Health got it right-less heroin needed to die when alcohol’s in the mix. Same applies here. You don’t need to be a heavy user. One beer. One shot. One night. That’s all it takes.
Carry naloxone. Know the signs. Ask your pharmacist. Don’t assume. Don’t guess. Don’t trust your gut. Your gut is not a pharmacologist.
Melania Rubio Moreno
December 1, 2025 AT 22:55ok but like… what if you just take one little hit of coke and a sip of wine? like… is that really that bad? i mean people have been doing it since the 80s
Shubham Semwal
December 3, 2025 AT 06:22lol you think you’re special? you think your body is different? you think your liver is a superhero? every single person who dies from this combo thought they were the exception. your body doesn’t care how cool you think you are. it just stops breathing. you’re not edgy. you’re just dead.
Leo Adi
December 3, 2025 AT 21:33My uncle died this way. Took his pain meds after a back surgery. Had a couple of beers with dinner. Fell asleep. Never woke up. They found him with his glass still in hand. No struggle. No noise. Just… gone. I didn’t know until after. That’s why I share this. Not to judge. Just so someone else doesn’t lose someone the way I did.
Sam HardcastleJIV
December 4, 2025 AT 09:26The structural paradox inherent in contemporary pharmacological discourse lies in the conflation of individual agency with systemic negligence. While the onus is placed upon the layperson to discern lethal interactions, the pharmaceutical industry and regulatory bodies have historically underprioritized the dissemination of synergistic toxicity data. The resultant epistemic deficit is not merely a failure of education-it is a failure of institutional responsibility.
Alex Hess
December 4, 2025 AT 09:43This is just fearmongering dressed up as public service. People have been mixing drugs since the dawn of civilization. The fact that you’re surprised people die from it says more about your naivete than their recklessness. Also, naloxone isn’t magic. It doesn’t work on benzos or alcohol. You’re just giving false hope.