Every year, 23,000 people end up in the emergency room because of interactions between dietary supplements and prescription medications. Many of these cases are preventable. The problem isn’t that supplements are inherently dangerous-it’s that most people don’t know what to ask before popping a pill alongside their heart medicine, antidepressant, or blood thinner.
You take vitamin D because your doctor said your levels are low. You grab turmeric for your knees. You start St. John’s wort because you read it helps with mild depression. But what if that turmeric increases your blood pressure meds’ side effects? What if the St. John’s wort makes your birth control useless-or worse, cancels out your HIV medication? These aren’t hypotheticals. They happen every day.
Why Supplements Aren’t Like Prescription Drugs
When you get a prescription, the FDA has already checked its safety, dosage, and how it interacts with other drugs. That’s not true for supplements. Under the Dietary Supplement Health and Education Act of 1994, companies don’t need to prove their products are safe or effective before selling them. There are over 85,000 supplement products on U.S. shelves right now. Only 3% of them have any documented interaction data with medications.
That means if you buy a bottle of ginkgo biloba or goldenseal, there’s no guarantee what’s actually inside-or whether it will interfere with your lisinopril, metformin, or warfarin. Labels can be wrong. One study found 70% of supplement labels misstate ingredient amounts. You think you’re taking 500 mg of milk thistle? You might be getting 200 mg-or 800 mg. That kind of inconsistency turns a simple question into a gamble.
St. John’s Wort: The Most Dangerous Supplement You’ve Probably Heard Of
St. John’s wort is the most common supplement linked to dangerous drug interactions. It doesn’t just mildly affect medications-it can slash their effectiveness by half or more.
Take cyclosporine, the drug transplant patients need to keep their bodies from rejecting new organs. St. John’s wort drops cyclosporine levels by 50-60%. That’s not a small drop. That’s a rejection risk. In HIV patients, it cuts indinavir levels by 57%. That means the virus can bounce back. For women on birth control, it increases the chance of pregnancy by 40-50%.
It doesn’t stop there. St. John’s wort can trigger serotonin syndrome when mixed with SSRIs like fluoxetine or sertraline. Symptoms? Confusion, rapid heartbeat, muscle stiffness, high fever. It’s rare-but deadly. Reddit users have documented over 140 cases between 2022 and 2023. One woman wrote: “I didn’t realize St. John’s wort would make my birth control fail. I got pregnant because of it. My doctor never mentioned this.”
Dr. Paul Offit, a top infectious disease expert, calls it “the most dangerous over-the-counter supplement because it interacts with more prescription drugs than any other.” And yet, it’s still sold next to the protein powder at your local grocery store.
What About Ginkgo, Vitamin E, and Other “Safe” Supplements?
People assume “natural” means safe. That’s the biggest myth in supplement use.
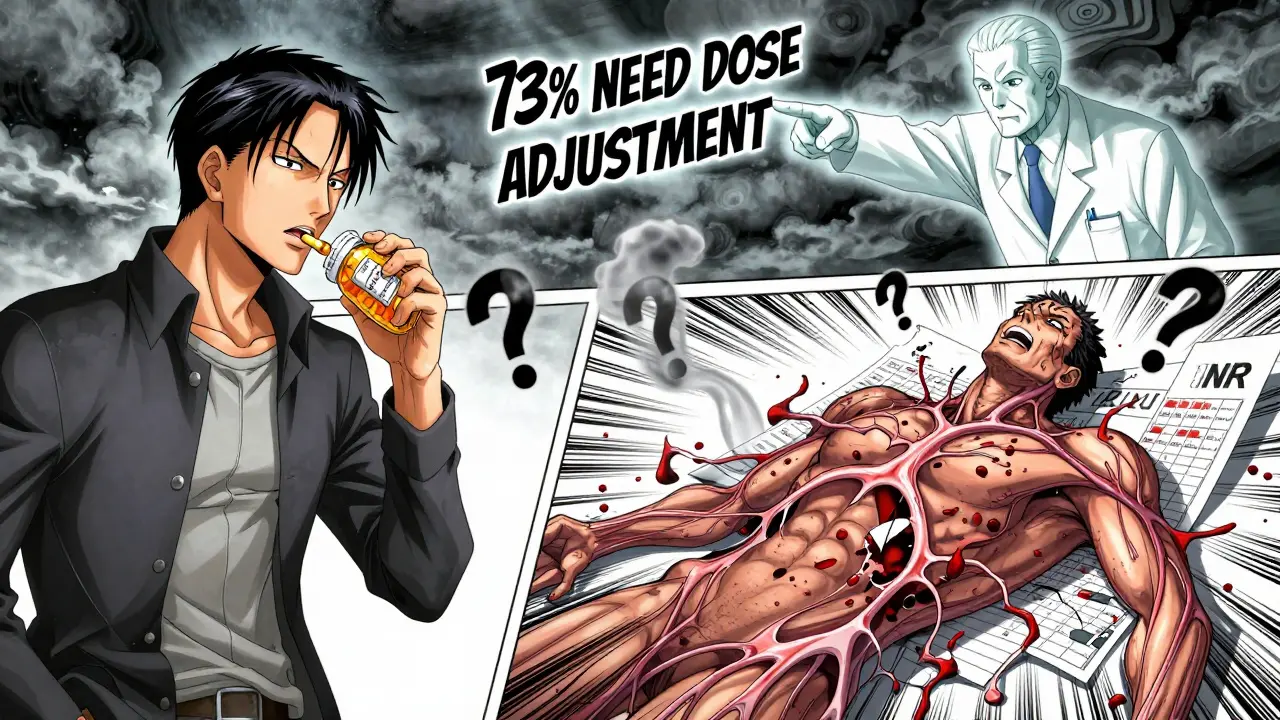
Ginkgo biloba is often taken for memory or circulation. But if you’re on warfarin, it’s a red flag. Studies show it can raise your INR (a blood clotting measure) to dangerous levels-2.5 to 3.5-in 15% of users. That’s the same range that puts you at high risk for internal bleeding. One study found 73% of warfarin patients taking ginkgo needed their dose adjusted. That’s not coincidence. That’s a direct interaction.
Vitamin E, especially in doses over 400 IU per day, can make warfarin stronger. It doesn’t just add to the effect-it can push your INR into the danger zone. A 2022 report from the NIH found it increases anticoagulation by 25-30%. That’s not a minor side effect. That’s a bleeding risk.
Even “mild” supplements like garlic, ginger, or fish oil can increase bleeding risk. If you’re scheduled for surgery, your doctor should know you’re taking them-even if you think they’re “just natural.”

Seven Questions to Ask Before Taking Any Supplement
You don’t need to be a pharmacist to protect yourself. Just ask these seven questions before adding any supplement to your routine.
- Does this supplement affect cytochrome P450 enzymes or drug transporters? St. John’s wort induces CYP3A4, a key enzyme that breaks down over 50% of all prescription drugs. If your medication is processed by this enzyme, the supplement can make it useless. Ask your pharmacist: “Is this supplement known to affect CYP3A4 or P-glycoprotein?”
- Could this create additive effects? If you’re on blood thinners, adding ginkgo, garlic, or high-dose vitamin E is like pouring gasoline on a fire. The effects stack. Same with sedatives-valerian root and melatonin can make you dangerously drowsy if mixed with benzodiazepines or opioids.
- Is there evidence this supplement reduces my medication’s effectiveness? Don’t guess. Look it up. St. John’s wort reduces digoxin levels by 25%. It lowers the effectiveness of antidepressants, birth control, and cancer drugs. If you’re on any of these, avoid it.
- Has this supplement been studied with my specific medication? Only 15% of supplements have formal interaction studies. If you’re on immunosuppressants, chemotherapy, or HIV meds, the risk is high and the data is scarce. When in doubt, skip it.
- What monitoring parameters should I track? If you’re on warfarin, your INR needs checking every few weeks. If you’re on HIV meds, your viral load should be monitored. If you start a new supplement, tell your doctor to check these numbers again. Don’t assume they’ll think of it.
- Are there safer alternatives? American ginseng has fewer interactions than Asian ginseng. Milk thistle has been studied with liver cancer drugs and, under supervision, may even help reduce side effects. Ask your pharmacist: “Is there a version of this supplement with a better safety profile?”
- What symptoms mean I’m having a dangerous interaction? Know the warning signs: confusion, rapid heartbeat, unexplained bruising or bleeding, sudden dizziness, nausea without cause, or a sudden change in how you feel on your meds. If you notice any of these after starting a supplement, stop it and call your doctor.
Who’s Responsible for This Gap?
It’s not just you. The system is broken.
Pharmacists now routinely screen for supplement interactions during medication reviews-89% do it. But only 32% of primary care doctors even ask about supplements in their charts. And when they do, the average conversation lasts 1.2 minutes.
The FDA can’t require safety testing for supplements. The industry spends $52 billion a year selling them. Only 3% have verified interaction data. Meanwhile, the CDC estimates supplement-related ER visits will rise unless education improves.
Some experts, like Dr. Pieter Cohen of Harvard, say this is a public health experiment-where consumers are the test subjects. Others, like the Council for Responsible Nutrition, argue serious interactions are rare. But rare doesn’t mean nonexistent. And when the stakes are organ rejection, HIV rebound, or a stroke from a bleed, “rare” is too risky.
What You Can Do Right Now
Here’s your action plan:
- Make a list of every supplement you take-name, dose, frequency.
- Bring it to your next doctor or pharmacist visit. Don’t wait for them to ask.
- Use the NIH’s LiverTox database or Drugs.com’s interaction checker to look up your specific combo.
- If you’re on warfarin, HIV meds, immunosuppressants, or cancer therapy, avoid St. John’s wort, goldenseal, and high-dose vitamin E entirely unless your doctor says otherwise.
- When in doubt, skip it. There’s almost always a safer way to support your health-through diet, sleep, movement, or proven medical treatments.
You don’t need to take every supplement on the shelf. You don’t need to trust marketing claims. You just need to ask the right questions-and then act on the answers.
Frequently Asked Questions
Can I take vitamin D with my blood pressure medication?
Yes, vitamin D generally doesn’t interfere with blood pressure medications like ACE inhibitors or beta-blockers. But if you’re also taking calcium supplements or have kidney disease, high doses of vitamin D can raise calcium levels, which may affect heart rhythm. Stick to the recommended dose (600-800 IU daily) unless your doctor orders otherwise.
Is it safe to take melatonin with antidepressants?
Melatonin is usually safe with SSRIs like sertraline or fluoxetine, but it can increase drowsiness. Avoid combining it with sedatives like benzodiazepines or opioids. There’s no strong evidence melatonin reduces antidepressant effectiveness, but if you feel unusually tired or foggy after starting it, talk to your doctor.
Why do some supplements say “may interact with medications” but don’t list which ones?
Because they’re not required to. Supplement labels don’t need FDA approval before being printed. The warning is often a legal disclaimer, not a detailed safety guide. If a label says “may interact,” assume it does-and check with your pharmacist before taking it.
Can I stop my supplement if I start a new medication?
Never stop or start anything without talking to your doctor or pharmacist. Some supplements can cause withdrawal effects, and stopping suddenly might trigger rebound symptoms. If you’re starting a new drug, pause the supplement until you’ve checked for interactions. Then decide together whether to restart it.
What should I do if I think a supplement is making my medication less effective?
Stop the supplement immediately and contact your provider. If you’re on blood thinners, HIV meds, or transplant drugs, don’t wait. Track symptoms: Are you feeling worse? Is your condition changing? Bring your supplement list to your next appointment. Your doctor may need to run a blood test to check drug levels or adjust your dose.
Are there any supplements that are proven safe with most medications?
Some have low interaction risk: American ginseng, cranberry (in juice form), and milk thistle (in controlled doses) have been studied and show fewer conflicts. But “low risk” doesn’t mean “no risk.” Always check with your provider, especially if you’re on multiple medications or have chronic conditions.
Can my pharmacist check for interactions for me?
Yes-and they should. Pharmacists are trained to spot supplement-drug interactions. Bring your entire list-prescriptions, over-the-counter meds, and supplements-to your pharmacy when you fill a new prescription. Ask: “Can you check these for interactions?” Most pharmacies offer this for free.




Liz MENDOZA
December 28, 2025 AT 09:38I used to take turmeric with my blood pressure meds without thinking twice. Then I started getting dizzy and my doctor had to adjust my dosage. Turns out, it was interacting. I wish someone had told me sooner. Now I always check with my pharmacist before trying anything new. Seriously, just ask. It takes two minutes and could save your life.
Elizabeth Alvarez
December 30, 2025 AT 07:14Let me tell you something they don’t want you to know. The FDA doesn’t regulate supplements because Big Pharma owns them. They make billions off prescription drugs and they’re terrified you’ll realize you can heal yourself with garlic and vitamin C instead of paying $800 for a pill that makes you sick. St. John’s wort? It’s been proven to work better than Prozac for depression. But the pharmaceutical lobby buried the studies. They don’t want you to know you can get off their drugs. The 23,000 ER visits? Probably caused by the side effects of the prescription meds, not the supplements. They’re just scapegoating natural remedies to keep you hooked. Wake up.
dean du plessis
December 31, 2025 AT 09:26Been on warfarin for 7 years and I take fish oil daily. My INR’s been stable. My doc knows. I don’t overthink it. Just keep it simple. Talk to your provider. Don’t panic. Most people are fine if they’re aware. No need to go full conspiracy or fear mode. Just be smart.
Caitlin Foster
January 1, 2026 AT 21:17Oh my god I can’t believe people still take St. John’s wort like it’s a harmless tea?? I literally had a friend get pregnant because she thought ‘natural’ meant ‘safe’ while on birth control. She cried for a week. And then she blamed the pill. NO. IT WAS THE HERB. I swear if I see one more person at the grocery store grabbing that stuff next to the protein powder I’m going to scream.
Alex Lopez
January 3, 2026 AT 00:45As a clinical pharmacist with 15 years of experience, I can confirm that the data cited in this post is accurate and underreported. The cytochrome P450 system is not a suggestion-it’s a biochemical highway. St. John’s wort induces CYP3A4 and P-glycoprotein with near-pharmaceutical precision. The 50-60% reduction in cyclosporine levels is not anecdotal-it’s documented in peer-reviewed transplant journals. I have seen patients reject kidneys because they took ‘natural mood support.’ This is not fearmongering. It is pharmacokinetics. Please, for the love of all that is holy, bring your supplement list to your pharmacist. We are trained for this. We are not here to judge. We are here to prevent death.
Monika Naumann
January 4, 2026 AT 08:00It is deeply concerning that Western societies glorify self-medication with unregulated substances. In India, we have centuries of Ayurvedic tradition, and even then, every herb is prescribed by a trained Vaidya after pulse diagnosis and dosha evaluation. You cannot simply buy a bottle of ginkgo and assume it is safe. This is not freedom. This is negligence. The FDA’s lax regulation is a symptom of a culture that confuses convenience with wisdom. If you are on medication, you owe it to yourself and your family to seek professional guidance-not Google.
Elizabeth Ganak
January 5, 2026 AT 00:41i just started taking milk thistle for my liver after my doctor said my enzymes were high and i was scared to ask because i thought theyd think i was weird but they were super chill about it and even checked the interaction with my metformin. turns out its fine! so just talk to someone. its not a big deal. theyve heard it all before.
Liz Tanner
January 6, 2026 AT 19:25I’m so glad this post exists. I used to roll my eyes at people who asked about supplement interactions-until my mom had a near-fatal bleed after adding high-dose vitamin E to her warfarin regimen. She didn’t know. No one asked. The ER doctor said, ‘This happens more than you think.’ Now I carry a printed list of my meds and supplements everywhere. I ask my pharmacist every time. I tell my friends. It’s not paranoia. It’s responsibility.
Babe Addict
January 7, 2026 AT 06:06Y’all are overreacting. CYP3A4 induction? P-glycoprotein? That’s just pharmacology jargon to scare people into buying more prescriptions. The real issue is that Big Pharma doesn’t profit from herbs. St. John’s wort has been used for millennia. The fact that it interacts with SSRIs means it’s working-your brain is responding. The real danger is pharmaceutical dependency. Also, vitamin E doesn’t ‘make warfarin stronger’-it just supports endothelial integrity. Your INR fluctuates anyway. Chill. Stop treating your body like a chemistry lab.
Kishor Raibole
January 8, 2026 AT 22:33It is a matter of profound cultural decay that individuals in the United States, a nation endowed with unparalleled medical infrastructure, would willingly ingest unregulated botanical compounds without consulting licensed professionals. The very notion that one may self-prescribe based on Reddit anecdotes or Instagram influencers constitutes a dereliction of civic and biological duty. The Dietary Supplement Health and Education Act of 1994, while well-intentioned, has devolved into a legal loophole enabling corporate exploitation of public ignorance. One must ask: Is the pursuit of convenience worth the potential for irreversible organ damage? The answer, in any rational society, is self-evident.
John Barron
January 10, 2026 AT 07:53As a former pharmaceutical rep, I’ve seen the numbers. The 3% of supplements with interaction data? That’s because the rest haven’t been studied-because no one’s paying for it. But here’s the real kicker: the FDA doesn’t ban anything unless it kills someone. So St. John’s wort stays on shelves until someone’s transplant fails. And then? They slap a tiny warning on the label and move on. I’ve seen people die because they thought ‘natural’ meant ‘no side effects.’ I’ve held their hands in the ICU. This isn’t about fear. It’s about legacy. Don’t be the person who took the supplement and left their family with a funeral bill and a question mark. 💔