When you hear the word meningitis, it might sound like just another illness. But this isn’t the kind of fever or stomach bug you can sleep off. Meningitis is inflammation of the protective layers around your brain and spinal cord - the meninges. It can strike fast, hit hard, and leave lasting damage if not caught early. The good news? We have tools to stop it - and they work.
What Causes Meningitis? Not Just One Thing
Meningitis isn’t one disease. It’s five different types, each with its own cause, speed, and severity. The most dangerous is bacterial meningitis. It’s caused by bacteria like Neisseria meningitidis (meningococcus), Streptococcus pneumoniae (pneumococcus), and Haemophilus influenzae type b (Hib). These bugs don’t just make you sick - they can kill within hours. Even with treatment, 5 to 30% of people die. Survivors often face hearing loss, brain damage, or learning problems. Then there’s viral meningitis. It’s far more common - about 85% of all cases. Most are caused by enteroviruses, the same viruses that give you a cold or stomach upset. This type usually isn’t life-threatening. People recover in about a week without special treatment. But it still lands you in the ER because the symptoms look terrifyingly similar to bacterial meningitis. Fungal meningitis is rare and mostly hits people with weak immune systems - like those with HIV, cancer, or on long-term steroids. The main culprit is Cryptococcus neoformans. It’s not contagious, but it’s deadly if missed. Parasitic meningitis? Even rarer. It comes from eating raw or undercooked snails or slugs, mostly in Southeast Asia and the Pacific Islands. And then there’s non-infectious meningitis, triggered by things like lupus, certain drugs, or cancer. It’s not spread from person to person, but it still needs quick diagnosis.What Are the Real Symptoms? (It’s Not Just a Stiff Neck)
You’ve heard the classic signs: fever, stiff neck, headache. But here’s the truth - only 41% of people with bacterial meningitis show all three. That’s why so many get misdiagnosed. In fact, 70% of patients have at least one of those symptoms, but the rest? They might just feel like they’ve been hit by a truck. Here’s what actually happens:- High fever - over 101.3°F (38.5°C) in 86% of cases
- Severe headache - reported by 87% of patients
- Neck stiffness - so bad you can’t touch your chin to your chest
- Light sensitivity - bright lights hurt your eyes
- Vomiting - often sudden and forceful
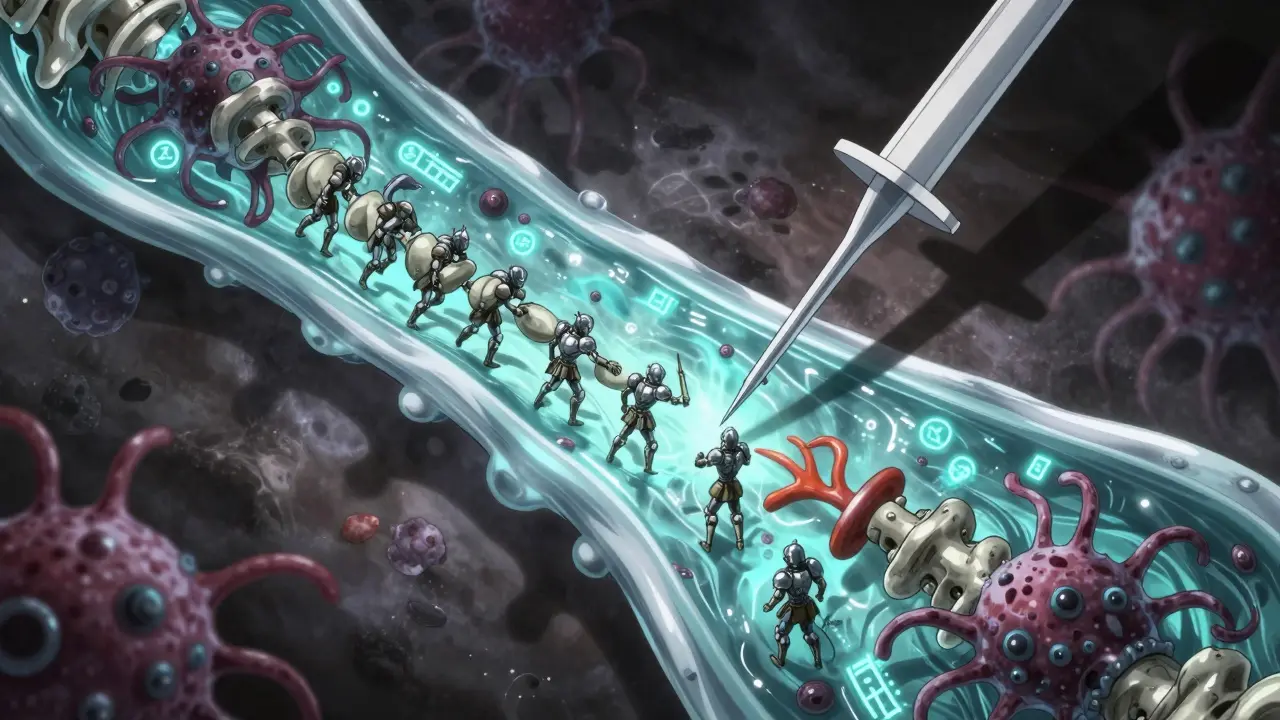
How Is It Diagnosed? It’s Not a Simple Test
You can’t diagnose meningitis with a rapid test or a home kit. It requires a spinal tap - a procedure where a needle draws fluid from your lower back. That fluid, called cerebrospinal fluid (CSF), tells the story. In bacterial meningitis, the CSF shows:- White blood cell count over 1,000 per microliter
- Low glucose (under 45 mg/dL)
- High protein (over 100 mg/dL)

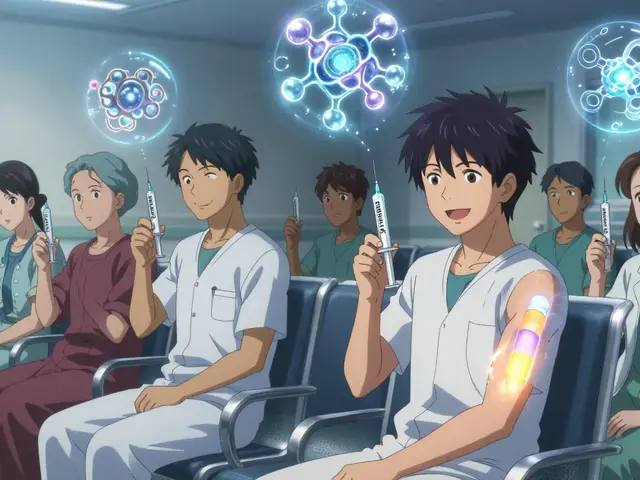
Vaccines: The Real Game-Changer
This is where things get powerful. Vaccines have turned meningitis from a death sentence into a preventable condition. For bacterial meningitis, there are three key vaccines:- MenACWY - protects against four types of meningococcus (A, C, W, Y). Recommended for all kids at age 11-12, with a booster at 16. It’s 80-85% effective. In the U.S., it prevents about 800 cases a year.
- MenB - targets serogroup B, the most common cause in teens and young adults. Two brands: Bexsero and Trumenba. It’s 60-70% effective. Since 2024, the CDC now recommends it for all adolescents, not just high-risk groups.
- PCV13 - pneumococcal vaccine for kids under 5. Reduces meningitis caused by pneumococcus by 80%.
- Hib - once a top cause of meningitis in children. Now, thanks to routine vaccination, cases have dropped by 99% in countries with full immunization programs.
What About Non-Vaccine Prevention?
Vaccines are the strongest shield, but they’re not the only one. Simple habits matter:- Wash your hands often - cuts transmission risk by 30-50%
- Don’t share drinks, utensils, or toothbrushes - reduces spread by 25%
- If you’re pregnant, avoid unpasteurized cheese and undercooked meat - this prevents listeria, which can cause meningitis in newborns
Why This Matters Right Now
New vaccines are coming. In early 2024, the WHO approved a low-cost MenACWY vaccine priced at just $0.50 per dose for use in Africa. That’s a game-changer for countries that can’t afford the $100+ doses used in the U.S. Also, a new universal meningococcal vaccine is in Phase II trials. Early results show 92% effectiveness against all serogroups. If it works, we could one day have one shot that protects against everything. But there’s a catch. Antibiotic resistance is rising. In the U.S., 32% of pneumococcal meningitis strains are now resistant to penicillin - up from 15% in 2010. That means doctors have to start with stronger, broader antibiotics right away, even before test results come back. The goal? The WHO’s "Defeating Meningitis by 2030" plan wants to cut cases by half and deaths by 70%. We’re on track - but only if vaccines reach everyone. Right now, 90% of meningitis deaths happen in low-income countries. That’s not just a health issue. It’s a justice issue.What Should You Do?
If you’re a parent: Make sure your child gets the MenACWY vaccine at 11-12 and the booster at 16. Ask about MenB - it’s now recommended for all teens. If you’re going to college: Many schools require proof of meningitis vaccination. If yours doesn’t, get it anyway. Dorm life increases your risk 3-5 times. If you’re sick and feel worse than a normal flu: Don’t wait for the rash. Don’t assume it’s just a headache. If you have fever, stiff neck, confusion, or vomiting - go to the ER. Time is everything. Meningitis doesn’t care if you’re young or old, rich or poor. But prevention? That’s in your hands. Vaccines work. Symptoms matter. And knowing the difference could save a life.Can you get meningitis more than once?
Yes, but it’s rare. Most people develop immunity after one infection. However, different types of meningitis are caused by different germs. So if you had viral meningitis, you can still get bacterial meningitis later. Vaccines protect against specific strains, not all types. That’s why staying up to date on shots matters even if you’ve had it before.
Do meningitis vaccines cause autism?
No. There is no link between meningitis vaccines and autism. This myth came from a discredited study from over 20 years ago that was retracted due to fraud. Since then, dozens of large studies involving millions of children have found no connection. The CDC, WHO, and every major medical group agree: vaccines are safe.
Is meningitis contagious?
Bacterial and viral meningitis can be contagious, but not in the way you think. You don’t catch it just by being near someone. It spreads through close contact - coughing, kissing, sharing drinks or utensils. Fungal, parasitic, and non-infectious types aren’t contagious at all. That’s why handwashing and not sharing personal items are so important.
Can adults get meningitis vaccines?
Absolutely. While vaccines are often given to kids, adults who missed them can still get them. MenACWY is recommended for anyone under 25 who hasn’t been vaccinated. MenB is especially important for college students, military recruits, and people with weakened immune systems. Even if you’re over 25, talk to your doctor - some adults need it based on health conditions or travel plans.
What if I don’t remember if I got the vaccine?
It’s better to get it again than risk being unprotected. Vaccines are safe to repeat. Your doctor can check your records, but if they’re lost, just get the shot. There’s no harm in an extra dose, and the protection is worth it. Many colleges and employers now require proof - so it’s worth sorting out.
Are meningitis vaccines free?
In the U.S., most insurance plans cover meningitis vaccines at no cost under the Affordable Care Act. Public health clinics and school-based programs often offer them for free or low cost. In Australia, the National Immunisation Program provides MenACWY and Hib vaccines for free to children and teens. MenB is not yet publicly funded but may be covered by private insurance. Check with your local health department or doctor.




Palesa Makuru
January 3, 2026 AT 07:42Ugh, I can't believe people still think meningitis is just 'a bad flu.' I had a roommate in Cape Town who ignored her headache for three days-turned out it was meningococcal. She lost her hearing in one ear. Vaccines aren't optional, they're basic human decency. If you're skipping them, you're literally gambling with other people's lives. 🤦♀️
Lori Jackson
January 4, 2026 AT 01:45Let’s be real-the real epidemic isn’t meningitis, it’s anti-vaxxer pseudoscience masquerading as 'personal freedom.' The CDC data is unequivocal: vaccines prevent 1,000+ cases annually in the U.S. alone. Yet we still have parents citing discredited studies from 2002 like they’re gospel. The cognitive dissonance here is staggering. We’ve eradicated Hib in developed nations through science, not superstition. Why are we still having this conversation in 2025?
Wren Hamley
January 4, 2026 AT 02:36Okay, but let’s nerd out for a sec-did you know the MenA vaccine in Africa is basically a miracle? $0.50 per dose, 99% drop in cases? That’s not just public health, that’s geopolitical poetry. Imagine if every vaccine rollout had that kind of ROI. And the new universal meningococcal vaccine in Phase II? If it hits 92% across serogroups, we’re looking at a world where meningitis becomes a footnote in medical textbooks. I’m not usually emotional about immunology, but this? This is hope in a vial.
Also, the fact that we’re still seeing penicillin resistance in 32% of pneumococcal strains? That’s a wake-up call for stewardship. We need to stop treating antibiotics like candy and start treating them like the last line of defense they are.
Sarah Little
January 5, 2026 AT 10:29Just read this whole thing. So many people don’t realize that viral meningitis still requires ER visits because it mimics bacterial. I had it sophomore year. Thought I had a migraine. Ended up in the hospital for 48 hours. They did the spinal tap. It hurt. I cried. I was 19. No one told me it could be this bad. Please just get the shots. Even if you think you’re invincible.
innocent massawe
January 5, 2026 AT 17:42Thank you for this. In Nigeria, many still think meningitis is a curse or punishment. I showed my cousin this article-he’s 24, never been vaccinated. He’s getting MenACWY next week. Small steps. 😊
veronica guillen giles
January 5, 2026 AT 17:58Oh wow, so now we’re giving teenagers a *choice* about vaccines? How quaint. Next you’ll be asking if they want to brush their teeth or if they’re feeling ‘vibes’ about tetanus. Let me guess-you also think the flu shot is ‘optional’ and that ‘natural immunity’ is some kind of spiritual upgrade? Sweetheart, the only thing natural about meningitis is the part where you die in a hospital bed while your parents beg for a miracle. Get. The. Shot.
erica yabut
January 6, 2026 AT 10:37MenB is only 60-70% effective? So… it’s basically a glorified placebo with a price tag? Why are we still pushing this like it’s the second coming? And why is everyone acting like this is new info? I’ve been screaming about this since 2018. Also, 'sore arm' my ass-my cousin got a 103 fever after MenB. You call that mild? 😒
Tru Vista
January 8, 2026 AT 10:03lol vaccines dont cause autism but they do cause fevers. also why are we vaccinating adults? who even is this for? also my cousin got meningitis and he never got a shot so…