Getting a medication dose wrong can kill. It’s not a hypothetical risk-it’s a daily reality in hospitals, clinics, and pharmacies. A decimal point misplaced. A handwritten '10U' misread as '1.0U'. A nurse rushing through a med pass during a 12-hour shift. These aren’t rare mistakes. They happen more often than most people realize. And when they do, the consequences are often irreversible.
The good news? Most of these errors are preventable. The key isn’t working harder-it’s working smarter. Verifying dose changes isn’t just a box to tick. It’s a safety system built on clear protocols, reliable tools, and honest communication. If you’re a nurse, pharmacist, or provider, this isn’t about following rules. It’s about protecting someone’s life.
Why Dose Verification Isn’t Optional
In 2022, over 1,200 reported incidents involved incorrect dose changes. Nearly 300 of those caused serious harm. The ECRI Institute ranked inadequate dose verification as the third biggest health technology hazard that year. These aren’t abstract stats-they’re real people. A child given ten times the intended insulin dose. An elderly patient on warfarin with an INR that spiked because no one checked the last lab result. A patient on heparin who bled internally because the pump was programmed wrong.
The Institute for Safe Medication Practices (ISMP) calls these high-alert medications: insulin, heparin, opioids, IV potassium, and others. A mistake with these drugs doesn’t just cause side effects-it causes cardiac arrest, respiratory failure, or death. And the biggest trigger for these errors? Miscommunication during transitions. When a doctor writes a new order, when a shift changes, when a patient moves from ICU to a floor. That’s when the handoff breaks down.
The Three-Step Verification Process
There’s no magic bullet. But there is a proven, step-by-step method that works across settings. The ISMP recommends a 3-step verification for every dose change, especially with high-alert drugs:
- Independent calculation - Two qualified providers calculate the dose separately. No talking. No looking at each other’s work. One does the math based on weight, renal function, or lab values. The other does the same. If the numbers don’t match, they stop. No exceptions. This takes 2-3 minutes, but it catches 90% of calculation errors.
- Context check - Now you cross-reference the dose with the patient’s current condition. Did their kidney function change? Are they on a new drug that interacts? Is their weight up or down? For warfarin, you need an INR result from the last 24 hours. For insulin, you need recent blood sugars. Skipping this step is like checking the tire pressure but ignoring the road conditions.
- Bedside verification with barcode scanning - Before you give the drug, scan the patient’s wristband. Scan the medication. The system should match the drug, dose, route, and time to the electronic order. If it doesn’t, you don’t proceed. This step alone prevents 86% of wrong-drug and wrong-dose errors, according to studies in the Journal of the American Medical Informatics Association.
It sounds simple. But in practice? It’s hard. Nurses are stretched thin. Systems glitch. Alerts go ignored. That’s why this process only works if it’s built into the workflow-not tacked on as an extra step.
Barcode Scanning vs. Human Double Checks
You’ll hear people argue: ‘Barcodes are better.’ Or ‘Human checks catch what machines miss.’ The truth? You need both. They’re not rivals-they’re partners.
Barcode medication administration (BCMA) systems are excellent at catching the obvious mistakes: wrong patient, wrong drug, wrong dose. A 2009 study showed BCMA prevented 86% of potential errors. But here’s the catch: if the barcode is scanned correctly but the dose is still wrong-because the concentration was entered wrong, or the order was miswritten-the system won’t flag it. That’s happened. A pharmacist once told me about a 10-fold insulin overdose that slipped through because the system saw ‘10 units’ as correct, even though the patient needed 1 unit.
That’s where independent double checks shine. A 2018 study found that when two nurses independently checked an IV heparin bag, they caught 100% of wrong-vial errors. Machines didn’t see it. The labels looked the same. Only human eyes caught the difference.
So here’s the rule: Use barcode scanning for patient, drug, and dose confirmation. Use human double checks for complex calculations, infusion pump settings, and high-alert drugs. Don’t pick one. Use both.
Communication Is the Missing Link
Here’s the dirty secret: 65% of serious medication errors linked to dose changes trace back to poor communication, according to The Joint Commission. It’s not that people are careless. It’s that we don’t have a common language.
Think about how often you hear:
- ‘Give him the usual insulin dose.’
- ‘He’s on 10 units.’
- ‘Just give what the chart says.’
These aren’t instructions. They’re invitations to error.
The fix? Use SBAR: Situation, Background, Assessment, Recommendation. It’s not fancy. It’s just structured.
Instead of saying: ‘Change his insulin,’ say:
- Situation: ‘Mr. Lee’s morning blood sugar was 320. He’s on sliding scale insulin.’
- Background: ‘He’s had consistent highs the last three days. His creatinine is stable. No new meds.’
- Assessment: ‘I believe he needs an increase from 8 to 10 units before breakfast.’
- Recommendation: ‘Can we change the order to 10 units before breakfast and recheck his glucose in 2 hours?’
That’s clear. That’s safe. That’s how you avoid miscommunication.
When Verification Fails-And Why
Even the best protocols fail when they’re not used right. Here’s what breaks them:
- Alert fatigue - Nurses get 15-20 alerts per shift. Most are false alarms. After a while, they start ignoring them. A 2022 study found only 15% of BCMA alerts were acted on during a 12-hour shift.
- Time pressure - During peak hours, 73% of nurses admit skipping verification steps. One nurse on Reddit wrote: ‘I had 8 patients, 3 were crashing, and I had 5 minutes to do med pass. I didn’t double-check insulin. I’m still haunted.’
- Wrong placement - Using double checks for every single dose? That’s not safety. That’s burnout. The ISMP says: ‘Don’t use double checks for everything.’ Save them for high-risk situations: insulin, heparin, opioids, pediatric doses, and when the order is handwritten.
- Poor documentation - If you don’t write down who verified, when, and what they checked, you can’t learn from mistakes. AHRQ found 29% of verification failures had incomplete records.
The solution? Stop treating verification as a checklist. Treat it as a culture. Give nurses 15-20 minutes per shift just for safety checks. Train with simulations, not PowerPoints. Celebrate when someone stops a mistake. Make it safe to speak up.

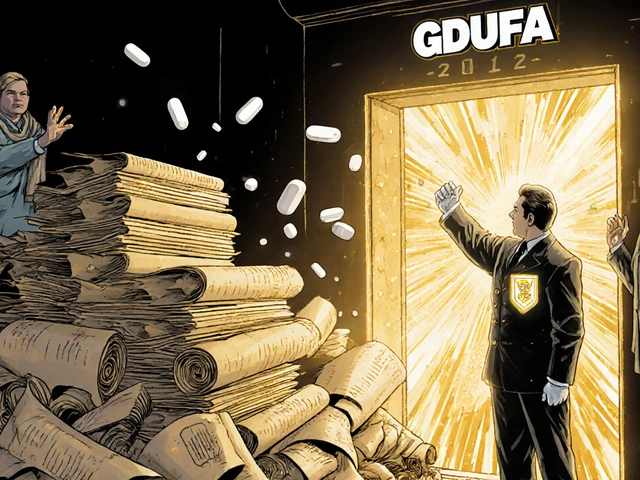
What’s Changing in 2025
Things are shifting. The Joint Commission now requires reliable dose verification processes under NPSG.01.01.01, effective January 2024. Hospitals that don’t comply risk penalties from CMS. The market for verification tech is growing fast-projected to hit $5.2 billion by 2027.
New tools are emerging:
- AI predictors - Epic’s DoseRange Advisor now flags unusual insulin or heparin orders based on patient history. In a 12-hospital trial, it cut inappropriate doses by 52%.
- Voice verification - Mayo Clinic is testing voice commands to log verifications. Nurses say it cuts documentation time by 65%.
- Blockchain logs - Some systems now create tamper-proof records of every dose change, who approved it, and when. Useful for audits and investigations.
But the biggest shift? Moving from universal double checks to targeted verification. Johns Hopkins Hospital redesigned their protocol to focus only on high-risk cases. Result? A 22% drop in errors-and nurses reported less stress. That’s the future: smarter, not busier.
What You Can Do Today
You don’t need a new system. You don’t need a budget. You need to start here:
- Ask before you give - If a dose change feels off, pause. Even if it’s ‘standard.’
- Use SBAR in handoffs - Especially during shift changes. 6-8 a.m. and 6-8 p.m. are the riskiest times. Don’t rush.
- Double-check high-alert meds - Insulin, heparin, opioids. Always. Even if you’ve done it a thousand times.
- Scan. Always. - If your facility has barcode scanning, use it. Every time.
- Document everything - Who verified? When? What did they check? If it’s not written, it didn’t happen.
Medication safety isn’t about perfection. It’s about layers. One person might miss something. Two might catch it. A system might fail. A human might stop it. When you combine verification with clear communication, you don’t just follow protocol-you save lives.



vinod mali
November 16, 2025 AT 13:07Been there. Saw a nurse almost give 10x insulin because the order said '10U' and the screen showed '10' without the U. We lost 20 minutes fixing it. Never skip the scan. Ever.
Jennie Zhu
November 17, 2025 AT 08:18It is imperative to underscore that the implementation of standardized verification protocols for high-alert medications constitutes a non-negotiable component of patient safety governance. The empirical data presented by the ECRI Institute and ISMP provide robust evidence for the institutionalization of dual independent verification procedures, particularly in contexts involving insulin, heparin, and opioid administration. Failure to adhere to these evidence-based practices represents a systemic vulnerability that may result in catastrophic iatrogenic harm.
Kathy Grant
November 17, 2025 AT 10:05I’ve sat in the quiet after a code call where the cause was a misread decimal. You don’t forget that. Not ever. I used to think double-checking was just procedure. Now I see it as a silent promise-to the patient, to their family, to yourself. It’s not about being perfect. It’s about refusing to let exhaustion win. That moment when you pause, even for 90 seconds, when something feels off? That’s where humanity still lives in this broken system. Keep doing it. Even when no one’s watching.
Robert Merril
November 17, 2025 AT 20:01Barcodes are great until the barcode is wrong and the system says its fine. I had a guy get 100mg of morphine because the order said 10mg and someone typed it wrong and the system didn’t catch it because it was within range. Machines are dumb. Humans are the only thing that can think. Stop trusting tech and start trusting your gut
Noel Molina Mattinez
November 18, 2025 AT 06:35Why are we still using paper orders in 2025? Someone needs to get fired for this. If you can’t type it you shouldn’t be writing it. And why do we still let nurses do math? That’s what pharmacists are for. This whole system is a joke
Roberta Colombin
November 19, 2025 AT 07:10Thank you for sharing this. I’ve worked in rural clinics where we didn’t have barcode scanners. We made our own checklists on sticky notes. It wasn’t perfect, but it kept people alive. Every step matters. Even the small ones. We all need to remember that safety isn’t about technology-it’s about care.
Dave Feland
November 19, 2025 AT 23:50Let’s be honest-this is all a controlled distraction. The real problem? Pharma companies push high-alert drugs because they make more money. The FDA is complicit. Hospitals don’t want to invest in real systems because it cuts into profit margins. You think this is about patient safety? It’s about liability and PR. The ‘three-step process’ is theater. The real solution? Ban all high-alert meds. But they won’t do that because the money’s too good.
Ashley Unknown
November 20, 2025 AT 10:29EVERYONE KNOWS THIS IS A TIME BOMB. I’ve seen nurses cry after giving the wrong dose. I’ve seen families lose children because someone was too tired to double-check. And what do they do? They give us another PowerPoint. They slap a sticker on the med cart. They say ‘we’re improving.’ But the shifts are still 12 hours. The staffing is still 1:8. The alerts still ignore you. And the next kid? The next elderly woman? She’s next. They don’t care. They just want to hit their metrics. This isn’t healthcare. It’s a death factory with a nice website.
Georgia Green
November 21, 2025 AT 17:37Just a heads up-when using SBAR, make sure you say ‘recommendation’ clearly. I had a resident say ‘change insulin’ and I thought they meant change the type, not the dose. Took 15 minutes to clarify. Write it down. Always. Even if you’re in a hurry. Your handwriting doesn’t matter. Your clarity does.
Christina Abellar
November 23, 2025 AT 11:44Scan. Double-check. Document. That’s it. No need to overcomplicate.
Margo Utomo
November 24, 2025 AT 19:12YES. This. 😭 I stopped a heparin error last week because I noticed the concentration didn’t match the order. The pump said 50 units/mL but the vial was 100. The barcode scanned fine. The system didn’t care. I asked the pharmacist. He said ‘oh yeah, we switched last night.’ No one told anyone. We need to stop pretending tech fixes everything. Humans still matter. 💪❤️
jalyssa chea
November 26, 2025 AT 02:56why do we even have nurses doing math? they cant even spell. i saw a chart once that said '10u' and the nurse read it as 100. no one checked. the patient died. why do we still let people who cant read write orders
Peter Stephen .O
November 26, 2025 AT 22:26Man, I’ve been in this game 18 years. Saw a kid get 10x insulin because the doctor wrote ‘10’ and the nurse thought it was ‘1.0’. We fixed it. Kid lived. But I’ll never forget the look on his mom’s face. Since then? I don’t trust my eyes. I don’t trust the screen. I don’t trust the system. I trust my hands. I check twice. I say it out loud. I scan. I write it down. And if someone says ‘we’re too busy’? I say ‘we’re too busy not to.’ This ain’t just procedure. This is how we keep each other alive.