Every year, millions of Americans throw away pills, creams, and liquids that still work-because they were stored wrong. It’s not just waste. It’s risk. Improper storage can turn your asthma inhaler into a dud, your insulin ineffective, or your antibiotics useless when you need them most. The medication storage habits most people follow-like keeping pills in the bathroom cabinet or near the stove-are actually making them expire faster. You don’t need fancy gear or a lab to keep your meds safe. You just need to know where not to put them, and where to put them instead.
Why Your Medicine Expires Sooner Than It Should
Expiration dates aren’t random. They’re based on real science. The FDA requires drugmakers to test how long a medication stays at 90-110% of its labeled strength under controlled conditions. That means if you store your medicine exactly how the manufacturer says, it should work until that date. But most people don’t. The CDC found that 37% of premature expirations happen because of bad storage-and humidity is the biggest culprit. Bathrooms? They’re the worst place in your house for meds. Showers spike humidity to 85-95%. That’s enough to break down aspirin 300% faster than normal. Heat does the same thing. Storing meds near the oven or on top of the fridge? Temperature swings of 15°C or more in just 30 minutes can ruin antibiotics, thyroid pills, and even pain relievers.
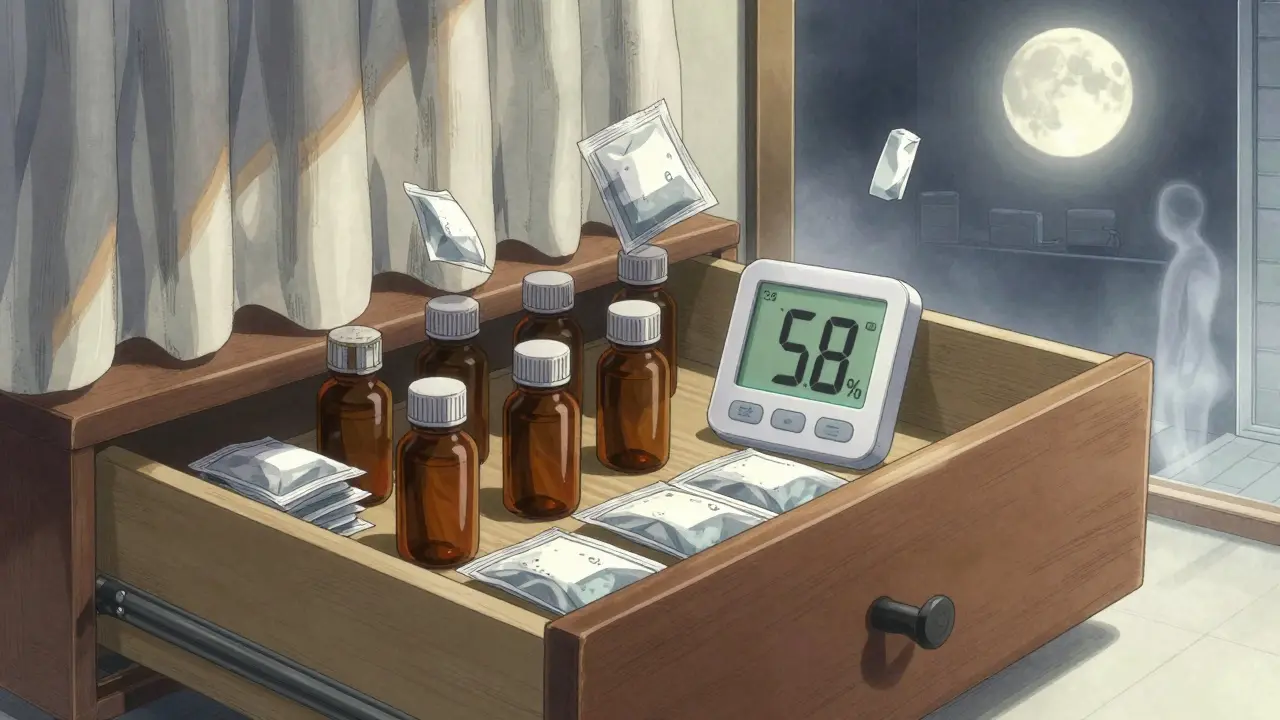
What the Perfect Storage Spot Looks Like
Forget the medicine cabinet. The best place for most pills and capsules is a cool, dry, dark spot-like a bedroom dresser drawer. Keep it away from windows, radiators, and anything that gets warm. The ideal temperature range is 20-25°C (68-77°F), with humidity below 60%. You don’t need a thermostat, but a simple digital hygrometer (under $15 online) can tell you if your drawer is safe. If it reads above 60%, move your meds. Some people use silica gel packs (the little white packets that come in new shoes or electronics) in their medicine drawer. They help soak up moisture and are safe if kept in a sealed container.
Keep It in the Original Bottle
That prescription bottle isn’t just for labels. It’s protection. Amber glass blocks 97% of UV light, which can break down drugs like nitroglycerin, certain antibiotics, and even birth control pills. Clear plastic containers? They offer almost no protection. If your pharmacy gave you meds in a clear bottle, transfer them to an amber glass container-many pharmacies will do it for free if you ask. And never dump pills into daily pill organizers unless you’re going to use them within a week. Long-term storage in those plastic trays exposes them to air and light, which speeds up degradation.
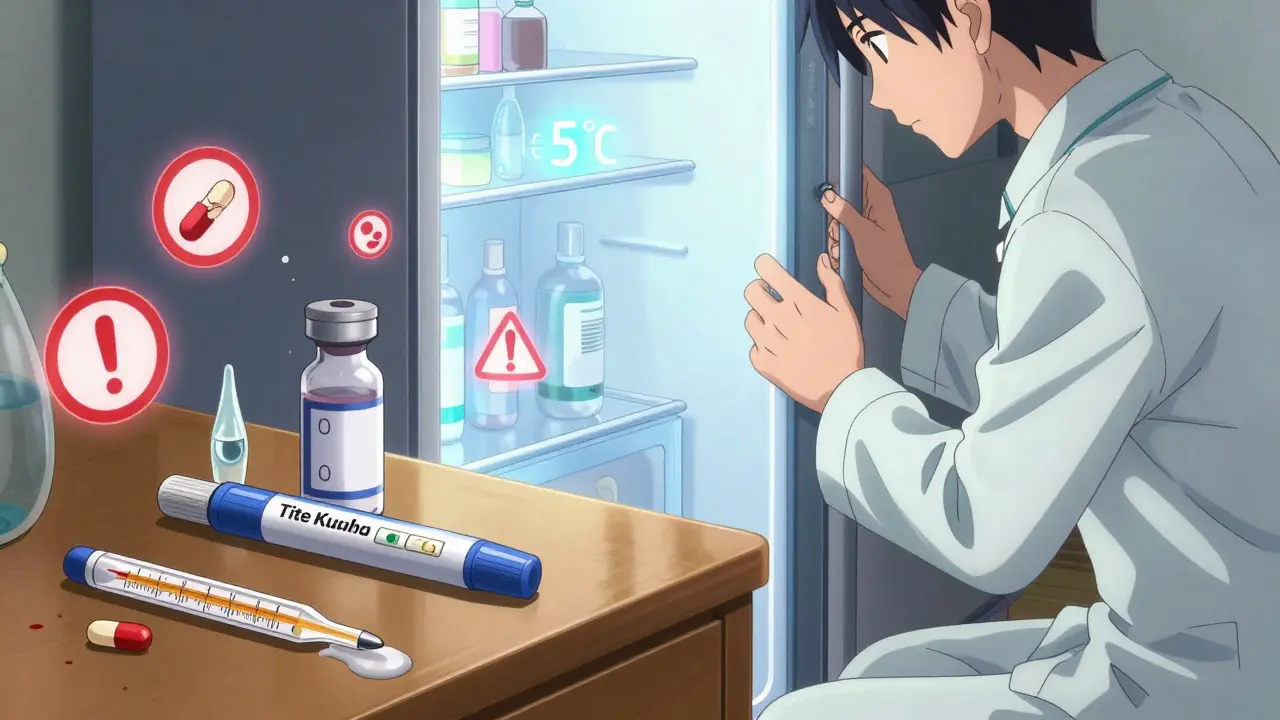
Refrigerated Meds: Don’t Guess, Know
Not all meds need the fridge. But some absolutely do. Insulin, certain eye drops, liquid antibiotics, and some biologics must be kept between 2-8°C (36-46°F). Put them in the center of the fridge-not the door. The door gets opened and closed constantly, causing temperature swings that can ruin them. Always check the label. If it says “refrigerate,” do it. But here’s the catch: once opened, some refrigerated meds can be kept at room temperature for a while. For example, insulin can last up to 28 days outside the fridge after first use. Don’t assume. Read the instructions. And never freeze anything unless it says you can. Freezing destroys the structure of many liquid medications.
Special Cases: What to Do With These
Some meds have unique rules. Nitroglycerin tablets-used for chest pain-must stay in their original dark glass bottle, tightly closed, away from light and heat. If you leave them out, they lose strength in days. Epinephrine auto-injectors (EpiPens) should be kept at room temperature, but never exposed to extreme heat or freezing. If your EpiPen turns cloudy or has particles, don’t use it. Eye drops are especially risky after expiration. A 2022 study found that 78% of expired eye drops were contaminated with Pseudomonas, a bacteria that can cause serious eye infections. Throw them out on the date listed-even if they look fine.
How to Track Expirations Before They Sneak Up
Most people don’t check expiration dates until they’re out of meds and reach for an old bottle. That’s too late. Set up a simple system. Pick one person in the household to do a monthly check. Go through every medicine, even the ones you haven’t used in months. Use colored dot stickers: red for this year, blue for next, green for two years out. That’s the method used by the University of Wisconsin, and it cut expired meds by 63% in their trial. Write the opening date on the bottle with a marker for things like eye drops or liquid antibiotics. Most last 28-30 days after opening. Mark it, and toss it after.
Signs Your Medicine Has Gone Bad
You don’t need a lab to tell if your medicine has degraded. Look for these red flags:
- Tablets or capsules that are discolored-more than 15% different from when you bought them
- Crumbly, cracked, or sticky pills
- Liquids that are cloudy, have particles, or smell off (aspirin that smells like vinegar is broken down)
- Eye drops that change color or become cloudy
- Insulin that looks grainy or clumpy after mixing
If you see any of these, don’t take it. Even if it’s before the expiration date. The degradation can happen faster than expected if stored poorly.
What to Do With Expired or Unwanted Meds
Never flush pills down the toilet or throw them in the trash where kids or pets can get them. The DEA runs National Prescription Drug Take Back Day twice a year-with over 11,000 collection sites across the country. Find your nearest drop-off location at dea.gov/takebackday. Many pharmacies also offer take-back bins. If none are available, mix pills with coffee grounds or cat litter in a sealed bag before tossing. It makes them unappealing and unusable. For liquids, pour them into a sealable container with kitty litter or sawdust. Don’t pour them down the drain.
New Tech Making Storage Easier
There’s new tech helping people store meds right. Smart pillboxes like the MedMinder Pro track temperature and humidity and send alerts if conditions go bad. Some pharmacies now include storage icons on labels-like a snowflake for refrigeration or a sun with a slash for avoiding heat. Merck released a new heat-stable insulin in late 2023 that stays effective at 30°C for 56 days-great for people without reliable refrigeration. And in 2025, the FDA plans to require real-time stability indicators on high-risk drugs. Until then, the best tool you have is awareness.
Why This Matters Beyond Saving Money
Wasting medication costs the U.S. $20 billion a year. But the real cost is health. Taking degraded antibiotics can lead to treatment failure and antibiotic resistance. A weak inhaler during an asthma attack could be life-threatening. Insulin that’s lost potency can cause dangerous blood sugar spikes. Proper storage isn’t about being neat-it’s about being prepared. Whether you’re managing a chronic condition, caring for an elderly parent, or just keeping a few painkillers on hand, getting this right saves money, prevents harm, and gives you peace of mind.
Can I store my medications in the bathroom?
No. Bathrooms are the worst place for most medications. Showers create high humidity-up to 95%-which breaks down pills and liquids faster. Heat from showers and hot water also causes temperature spikes. Even if your cabinet looks clean, the environment is damaging your meds. Store them in a cool, dry place like a bedroom drawer instead.
Do all medications need to be refrigerated?
No. Only specific ones do: insulin, some liquid antibiotics, certain eye drops, and biologics. Check the label or ask your pharmacist. Most tablets and capsules are fine at room temperature. Refrigerating them unnecessarily can cause condensation when you take them out, which might damage the pills. Don’t guess-follow the instructions.
Is it safe to use medicine after the expiration date?
Generally, no. While some studies show certain drugs stored perfectly may still work past expiration, those conditions don’t exist in most homes. Humidity, heat, and light degrade medications quickly. For critical meds like insulin, epinephrine, or antibiotics, using expired ones can be dangerous. Even for pain relievers, potency drops over time. If it’s expired, replace it.
What should I do if my medicine looks or smells weird?
Stop using it immediately. Discoloration, cracking, stickiness, cloudiness, or odd smells like vinegar (in aspirin) mean the drug has broken down. Even if it’s before the expiration date, it may not work-or could cause harm. Dispose of it safely and get a new prescription.
How can I keep track of expiration dates easily?
Use colored dot stickers: red for this year, blue for next, green for two years out. Do a monthly check with one person in your household responsible for it. Write the opening date on bottles for liquids and eye drops-most last only 28-30 days after opening. A quick 5-minute check each month prevents surprises.