Every year, hundreds of thousands of people in the U.S. get the wrong medication, the wrong dose, or wrong instructions at the pharmacy. Most of these mistakes aren’t caused by reckless pharmacists-they happen because the system is built to trust paperwork, not people. You walk in, hand over a prescription, and assume everything’s fine. But what if the label says 10 mg when the doctor meant 5 mg? What if you’ve been taking blood pressure pills for years, and this new bottle has a different color? What if the pharmacist grabs the wrong bottle because two drugs look alike? These aren’t rare accidents. They’re preventable. And you don’t need to wait for the pharmacy to fix it-you can protect yourself right now.
Why You Need a Personal Safety Checklist
Pharmacies are busy. Pharmacists are overworked. Prescription errors happen more often than you think. A 2022 study in the Journal of the American Pharmacists Association found that about 1 in 20 prescriptions filled in community pharmacies had at least one error-some minor, some dangerous. And here’s the thing: most of those errors were caught before they hurt anyone. Not by a computer, not by a second pharmacist. By the patient.You’re the only person who knows your body, your history, and your routine. No algorithm can replace that. A simple checklist doesn’t make you suspicious. It makes you smart. It’s not about doubting your pharmacist-it’s about adding a layer of safety that the system doesn’t provide.
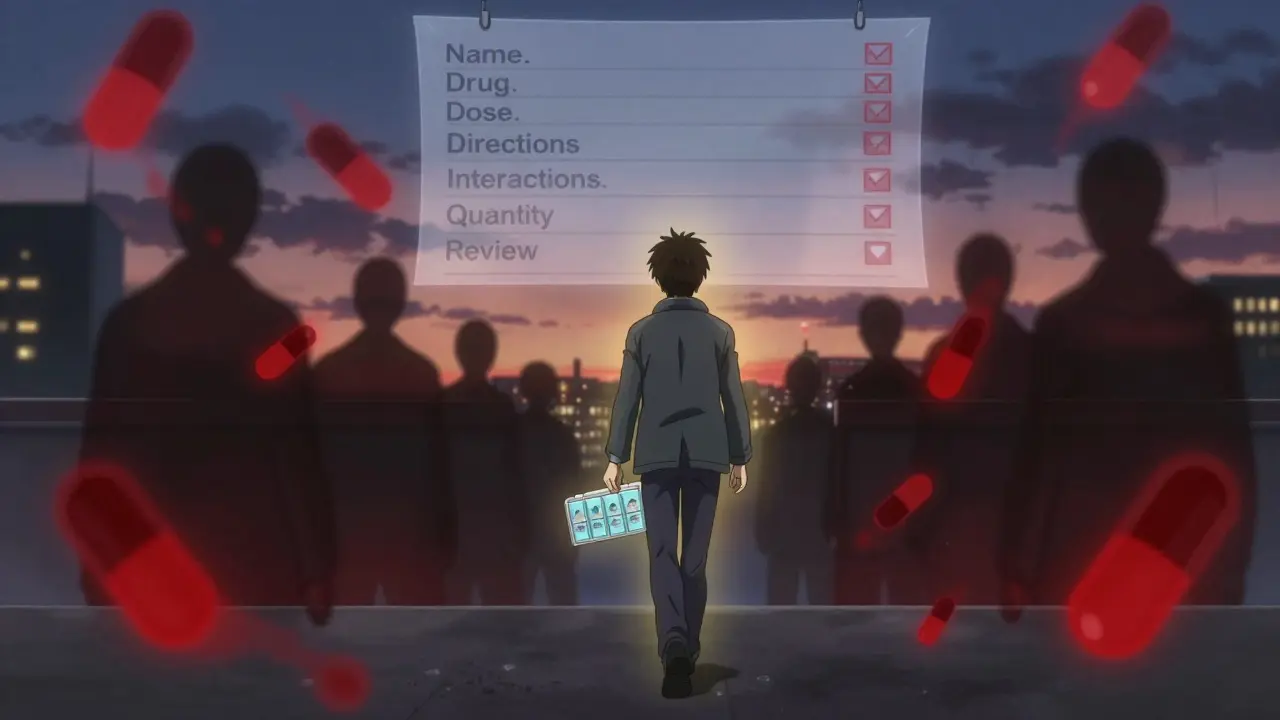
Your Personal Pharmacy Safety Checklist
Here’s what you should check every single time you pick up a prescription. Do this before you leave the counter.- Match the name on the bottle to your full legal name. Not just your first name. Not your nickname. Your full name as it appears on your ID. If it says “J. Smith” and you’re Jennifer Marie Smith, ask. This catches mix-ups with people who have similar names.
- Confirm the drug name. Read the name on the label out loud. Then say the name your doctor gave you. If they say “Lisinopril” and you expected “Zestril,” ask if they’re the same. Many drugs have brand and generic names. Don’t assume.
- Check the strength and dosage. Look for numbers like “5 mg,” “10 mg,” or “500 mg.” Compare it to your old prescription or your doctor’s instructions. If the number changed without you being told, pause. Ask: “Is this the same dose I was on before?”
- Verify the directions. Read the instructions: “Take one tablet by mouth twice daily.” Does that match what your doctor said? If they told you to take it with food and the label says “on empty stomach,” speak up. Misread directions are one of the top causes of adverse reactions.
- Compare pill appearance. If you’ve taken this medicine before, look at the shape, color, and markings on the pill. If it looks different, ask: “Is this the same medication?” Pills change manufacturers often, and sometimes the look changes dramatically. A white oval might become a blue capsule. That’s normal-but you should know why.
- Ask about interactions. Say: “I’m also taking [list your other meds]. Are there any risks with this new one?” Don’t wait for them to ask. Many pharmacists don’t know your full list unless you tell them. Even if you use the same pharmacy, they might not have your complete history.
- Confirm the quantity. Did they give you 30 pills? Or 90? If your prescription was for a 30-day supply and you got 90, ask why. Sometimes it’s a mistake. Sometimes it’s intentional-but you deserve to know.
- Request a verbal review. Say: “Can you walk me through what this is for and how to take it?” Most pharmacists will do this gladly. If they seem rushed, say: “I’d feel better if we took a minute to go over this.” You’re not being difficult. You’re being responsible.
What to Do If Something Feels Off
You don’t have to accept a wrong prescription. If anything on the checklist raises a red flag, stop. Don’t just say “I’ll check with my doctor later.” That’s too late.Here’s what to do:
- Ask the pharmacist to double-check the prescription with the prescriber’s office. Most pharmacies will do this on request.
- Ask to see the original prescription printout. Pharmacies keep a copy. You have the right to review it.
- If the pharmacist dismisses your concern, ask to speak to the manager. Pharmacists are trained to handle questions-no one should make you feel silly for asking.
- If you still feel unsure, don’t take the medication. Go to another pharmacy. Many will fill the same prescription without issue if the first one was wrong.
One woman in Ohio went to her pharmacy for her diabetes medication. The bottle said “Metformin 1000 mg.” She’d been on 500 mg for five years. She asked about it. The pharmacist said, “It must be a mistake.” They called the doctor. Turns out, the electronic prescription had been entered wrong. The dose would’ve caused severe lactic acidosis. She saved her own life by asking.
Prepare Before You Go
Don’t wait until you’re at the counter to think about this. Do a little prep work.- Keep a written list of all your medications. Include name, dose, why you take it, and how often. Update it every time your doctor changes something. Keep a copy in your wallet and on your phone.
- Take photos of your pill bottles. When you get a new prescription, snap a picture of the label and the pills inside. Store it in your phone. Next time, you can compare.
- Bring your old bottles. If you’re switching medications, bring the empty bottle from your last fill. It helps the pharmacist confirm the history.
- Use a pill organizer with labels. Even if you don’t need one, using it gives you a visual cue. If a pill doesn’t fit the slot, you’ll notice.
What Pharmacists Won’t Tell You
Most pharmacists want you to be safe. But they’re not trained to expect you to verify their work. In fact, many pharmacy systems are designed to assume the patient won’t question anything. That’s why:- They rarely ask you to confirm your date of birth unless it’s a controlled substance.
- They don’t always explain why a drug changed form (e.g., tablet to liquid).
- They may not know about supplements or over-the-counter meds you’re taking unless you mention them.
That’s not negligence. It’s system design. Your job isn’t to fix the system. It’s to protect yourself within it.
Real-Life Examples That Could’ve Been Prevented
- A man in Florida took his wife’s heart medication by accident. Same bottle size. Same color. He didn’t check the name. He ended up in the ER.
- A teenager was given a high-dose antidepressant instead of her ADHD medicine. The pharmacist confused the names. The girl had never taken antidepressants before. She called her mom immediately. She asked: “Is this right?”
- An elderly woman in Illinois got a new blood thinner. The label said “Warfarin 5 mg.” She’d been on 2 mg for years. She didn’t ask. She took it. Two days later, she had internal bleeding. She survived-but only because she went to the hospital.
Each of these could’ve been stopped by one simple question: “Is this what I’m supposed to get?”
What to Do After You Get Your Meds
Your safety doesn’t end at the door.- Check your pills within 24 hours. Compare them to your photo or old bottle.
- Watch for side effects. If something feels off-dizziness, rash, nausea, confusion-call your pharmacist. Don’t wait for it to get worse.
- Update your medication list. Write down the new drug, dose, and date you started.
- Set a phone reminder. If you’re starting a new med, set a 3-day reminder to ask: “Am I feeling different?”
When to Seek Help Beyond the Pharmacy
If you’ve been given the wrong medication and it caused harm-or if the pharmacy refuses to correct a clear error-don’t stay quiet.- Contact the Food and Drug Administration (FDA) through their MedWatch program. You can report errors online. It helps track patterns.
- File a complaint with your state’s Board of Pharmacy. They investigate dispensing errors.
- Ask your doctor to send a formal letter to the pharmacy. Sometimes a note from a prescriber gets results.
These steps aren’t about blaming. They’re about making sure this doesn’t happen to someone else.
You’re Not Overreacting
Some people think asking questions makes them a hassle. It doesn’t. It makes you the most important part of your own care. The pharmacy system was built to move fast. You’re the only one who can slow it down when it matters.Don’t wait for a mistake to happen. Start using this checklist today. Keep it on your phone. Print it out. Tape it to your wallet. The next time you walk up to the counter, you won’t just be picking up medicine. You’ll be preventing a mistake.
Do I really need to check every time, even if I go to the same pharmacy?
Yes. Even the best pharmacies make mistakes. Staff change. Systems glitch. Prescriptions get misread. A pharmacy that’s never made an error in five years can still hand you the wrong pill tomorrow. Consistency doesn’t eliminate risk-it just makes you complacent. Checking every time is the only way to stay safe.
Can I ask to see the original prescription?
Yes. You have the legal right to see the prescription that was sent to the pharmacy. Ask the pharmacist to pull up the electronic copy or printed version. Compare the drug name, dose, and instructions. If it doesn’t match what you were told by your doctor, the pharmacy can call the prescriber to clarify.
What if the pharmacist gets upset when I ask questions?
A good pharmacist will appreciate your caution. If they get defensive, ask to speak to the manager. If the manager is dismissive, go to another pharmacy. Your safety matters more than their ego. Many pharmacies compete for customers-use that. If one treats you like a burden, another will treat you like a priority.
Should I bring a list of all my supplements and OTC meds?
Always. Supplements like St. John’s Wort, garlic, or ginkgo can interact with prescription drugs. Even common things like aspirin or antacids can cause problems. Most pharmacists don’t ask unless you tell them. Bring your list. Write it down. Show it to them. It’s not extra-it’s essential.
Is there a way to reduce the number of pharmacy visits to lower risk?
Yes. Ask your doctor and pharmacist about mail-order prescriptions or 90-day fills. Fewer trips mean fewer chances for errors. Also, consider using one pharmacy for all your prescriptions. That way, they can check for interactions across all your meds. One pharmacy, one record, one safety net.
Next Steps
Start today. Print out this checklist. Put it in your wallet. Set a reminder on your phone: “Check meds at pharmacy.” Do it once. Then again next time. Soon, it’ll be automatic. You won’t be paranoid. You’ll be prepared.Medication safety isn’t a job for pharmacists alone. It’s a team effort. And you? You’re the captain.




Paula Sa
February 8, 2026 AT 17:27This is so needed. I’ve had two near-misses at the pharmacy-once with a blood thinner, once with an antibiotic. I always ask about the pill color now. It’s weird how many people just take it and go. You’re not being difficult-you’re being alive.
Natasha Bhala
February 9, 2026 AT 23:21Yesss. I keep a photo of every med bottle on my phone. Last month I caught a wrong dose because the pill looked different. Pharmacist apologized. Said they never thought anyone would notice. I’m just glad I did.
Mark Harris
February 9, 2026 AT 23:30THIS. My grandma almost died because she didn’t ask. She trusted the system. It didn’t trust her. Now she carries this checklist in her purse. I printed 10 copies. Gave them to all her friends. You’re not paranoid. You’re prepared.
AMIT JINDAL
February 11, 2026 AT 02:24LMAO i was just at the pharmacy yesterday and the girl handed me my med and i was like ‘wait is this 10mg or 5mg??’ and she was like ‘uhhh let me check’ and i was like ‘ok cool thanks for the 5 min delay’ 😂. But honestly? She was nice. We laughed. I think she’s gonna start asking patients if they want a ‘safety check’ now. I’m basically a pharmacy superhero. 🦸♂️
Tola Adedipe
February 12, 2026 AT 12:26I work in a pharmacy. We’re understaffed. We’re rushed. We make mistakes. But we also want you to ask. We’re not mad when you question us-we’re relieved. The ones who don’t ask? That’s the scary part. You think we like handing out 10x doses? No. We hate it. So please. Ask. We’ll thank you later.
Jesse Lord
February 13, 2026 AT 18:26I used to think this was overkill. Then my dad had a stroke because they gave him the wrong blood pressure med. He didn’t question it. He just took it. Now I carry this checklist in my wallet. I hand it to the pharmacist. I say ‘I’m not doubting you-I’m protecting us.’ They always pause. Then they smile. And they do it right.
Catherine Wybourne
February 14, 2026 AT 22:19I’m British, and I used to think Americans were weird for asking so many questions. Then I saw a friend nearly die because she didn’t. Now I ask my pharmacist if she’s had coffee today. If she says no, I say ‘Then let’s go over this slowly.’ She laughs. Then she does it. Turns out, a little sass saves lives.
Mary Carroll Allen
February 15, 2026 AT 04:30I’m a nurse. I’ve seen what happens when people don’t check. I’ve seen the ER reports. I’ve held the hands of people who didn’t ask. Please. Just. Ask. You don’t need to be loud. Just say ‘Can you confirm this is what my doctor ordered?’ That’s it. That’s all it takes. I’m begging you.
Amit Jain
February 15, 2026 AT 23:46OMG this is so basic. Of course you check. Of course you ask. Why is this even a thing? The system is broken. We’re not supposed to be our own pharmacists. But we are. Because no one else will. And if you don’t do this? You’re just lucky. Not smart. Stop being passive. Start being a human.
Niel Amstrong Stein
February 16, 2026 AT 01:56Been doing this for years. I even take pics of the label and the pill. I compare them every time. I’ve caught 3 errors. One was a kid’s asthma med swapped with a diabetes pill. I told the pharmacist. She cried. Said she’d been working 14 hours. I hugged her. We got coffee. Now she calls me ‘The Pill Detective.’ 😎
Marcus Jackson
February 17, 2026 AT 07:32you guys are overthinking this. if you’re on the same meds for 5 years, the pharmacy has your file. they’re not gonna mess it up. this checklist is for people who don’t know what they’re taking. if you’re responsible, you don’t need it. just trust the system.
Paula Sa
February 17, 2026 AT 11:23That’s the dangerous part, isn’t it? Trusting the system. Because the system doesn’t care if you live or die. It cares if the barcode scanned. It doesn’t care if the pill looks different. It doesn’t care if you’ve been on 5mg for a decade. It just processes. That’s why we have to care. And we do.
Eric Knobelspiesse
February 18, 2026 AT 10:16you’re all ignoring the root issue. it’s not about the checklist. it’s about capitalism. pharmacies are profit-driven. they want you to refill fast. they don’t want you to ask questions. they want you to be silent. this checklist? it’s a bandaid. the real fix? defund the system. rebuild it. but no one wants to hear that.
Ritu Singh
February 18, 2026 AT 22:33As someone from India, I’ve seen how medication safety is handled differently here. In rural clinics, patients are rarely given labels. They’re told orally. That’s why I now teach this checklist to my nieces and nephews. It’s not just safety-it’s empowerment. You are the last line of defense. And that’s not a burden. It’s a gift.
Joey Gianvincenzi
February 20, 2026 AT 14:35While I commend the intent of this checklist, it is imperative to note that such ad hoc measures are symptomatic of systemic regulatory failure. The FDA, state boards, and pharmacy licensing bodies must be held accountable for permitting such a fragile, human-dependent safety net. This is not patient empowerment-it is institutional abdication. We must demand structural reform, not behavioral compliance.