Understanding Pulmonary Arterial Hypertension and Rheumatoid Arthritis
Before diving into the connection between pulmonary arterial hypertension (PAH) and rheumatoid arthritis (RA), it's essential to understand what these two conditions entail. PAH is a rare but severe type of high blood pressure that affects the arteries in the lungs and the right side of the heart. It can lead to shortness of breath, fatigue, and chest pain, among other symptoms. On the other hand, RA is an autoimmune disease that primarily affects joints, causing inflammation, pain, and stiffness. So, what ties these two seemingly distinct conditions together? Let's explore their connection further.
How Rheumatoid Arthritis Can Lead to Pulmonary Arterial Hypertension
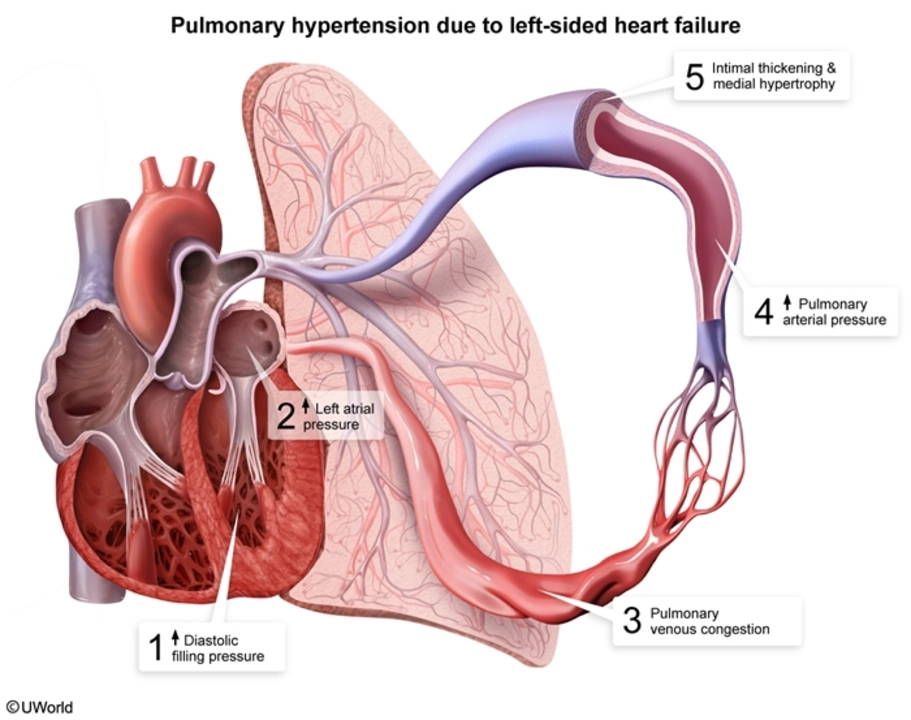
Rheumatoid arthritis is known to affect not only the joints but also other organs and systems in the body. One of these systems is the respiratory system, which includes the lungs. When RA causes inflammation in the lungs, it can damage the blood vessels and lead to PAH. This damage can cause a restriction in blood flow, making the heart work harder to pump blood through the narrowed arteries. The increased workload on the heart can eventually lead to heart failure if left untreated.
Recognizing the Symptoms of PAH in RA Patients
It is crucial to recognize the symptoms of PAH in patients with rheumatoid arthritis, as early detection and treatment can help manage the condition better. Some common symptoms of PAH in RA patients include shortness of breath, fatigue, dizziness, chest pain, and swelling in the ankles or legs. These symptoms may worsen over time, making daily activities more difficult. If you have RA and experience any of these symptoms, it's essential to consult your doctor for further evaluation and management.
Diagnosing Pulmonary Arterial Hypertension in Rheumatoid Arthritis Patients
Diagnosing PAH in RA patients can be challenging, as the symptoms may mimic other conditions. However, several tests can help determine if a patient with RA has developed PAH. These tests may include chest X-rays, echocardiograms, pulmonary function tests, and right heart catheterization. It is essential to discuss any concerns you have with your doctor, who can determine the appropriate tests and guide you through the diagnostic process.
Treatment Options for Managing PAH in Rheumatoid Arthritis Patients
While there is no cure for PAH, various treatment options can help manage the condition and improve the quality of life for those living with both RA and PAH. These treatments may include medications to relax the blood vessels, diuretics to reduce fluid buildup, and blood thinners to prevent blood clots. In some cases, more advanced treatments such as oxygen therapy or surgical interventions may be necessary. It is essential to work closely with your healthcare team to develop a personalized treatment plan that best addresses your needs.
Preventing Pulmonary Arterial Hypertension in Rheumatoid Arthritis Patients
While it may not be possible to prevent PAH entirely in patients with rheumatoid arthritis, some steps can help reduce the risk and improve overall health. These steps may include maintaining a healthy weight, exercising regularly, avoiding smoking, and managing RA through proper medication and lifestyle adjustments. Additionally, it's crucial to monitor your symptoms and communicate any changes or concerns to your healthcare team, helping to ensure that potential complications are addressed promptly.
Living with Rheumatoid Arthritis and Pulmonary Arterial Hypertension
Managing both rheumatoid arthritis and pulmonary arterial hypertension can be challenging, but with the right support and care, patients can maintain a good quality of life. It's essential to work closely with your healthcare team to manage your symptoms, adhere to your treatment plan, and make necessary lifestyle adjustments. Additionally, reaching out to support groups and connecting with others who share similar experiences can provide valuable emotional support and understanding during this journey.



Brendan Peterson
June 4, 2023 AT 10:36Most guidelines still treat it as a secondary issue, but it's the leading cause of death in seropositive RA patients after 10 years. If you're on methotrexate and getting winded climbing stairs, don't wait for a referral.
Jessica M
June 5, 2023 AT 20:26Erika Lukacs
June 7, 2023 AT 13:21Rebekah Kryger
June 7, 2023 AT 19:02Also, why do we assume inflammation causes PAH? What if it’s the other way around? Maybe PAH triggers systemic inflammation?
Just saying. Nobody’s proven causality. Just correlation with a fancy echo machine.
Victoria Short
June 8, 2023 AT 12:45Eric Gregorich
June 9, 2023 AT 05:25We don’t need more tests. We need to stop pretending the body is a machine with replaceable parts. It’s a living, furious, grieving thing-and when you ignore its whispers, it learns to scream in languages you can’t unhear.
Koltin Hammer
June 11, 2023 AT 02:31My cousin had both. She was 42. She didn’t complain until she couldn’t carry groceries. Then she was on oxygen in six months.
We need to screen RA patients like we screen for heart disease. Not because it’s trendy. Because it’s inevitable if we don’t.
Phil Best
June 12, 2023 AT 03:13Let me guess-someone finally noticed that autoimmune disease doesn’t stop at the synovium?
Newsflash: your immune system doesn’t read textbooks. It doesn’t care if you’re ‘only’ treating the knees. It’s a rogue empire with a vendetta.
And now you’re surprised the lungs are on fire?
Next up: ‘The Shocking Connection Between RA and Kidney Failure.’
Subscribe for Part 2.
Parv Trivedi
June 13, 2023 AT 07:19Willie Randle
June 14, 2023 AT 17:48PAH is not rare in RA. It’s underdiagnosed. And every month you delay, you lose lung reserve you can never get back.
Connor Moizer
June 16, 2023 AT 06:07It’s not optional. It’s not ‘maybe.’ It’s standard of care.
And if you’re on biologics? You’re at higher risk. So stop acting like you’re being proactive if you’re just taking pills and ignoring your lungs. You’re not managing RA-you’re just delaying the inevitable.
kanishetti anusha
June 17, 2023 AT 12:09roy bradfield
June 17, 2023 AT 14:08And the FDA? They’ve been in bed with Big Pharma since the 90s.
They don’t test for vascular damage because if they did, they’d have to recall half the arthritis drugs on the market.
So they give you a new pill. And another. And another.
Meanwhile, your lungs turn to dust.
And you? You think you’re getting better.
You’re not. You’re just being slowly sold out.