Hospital Discharge: What You Need to Know Before Leaving the Hospital
When you leave the hospital, you're not done with care—you're just switching settings. Hospital discharge, the process of transitioning a patient from inpatient care to home or another care setting. Also known as patient release, it’s one of the most dangerous moments in healthcare if nothing goes wrong—because too often, something does. Nearly 1 in 5 Medicare patients ends up back in the hospital within 30 days, and a big reason? Poor discharge planning. It’s not about being discharged too early—it’s about being left without clear instructions, the right meds, or someone to call when things go sideways.
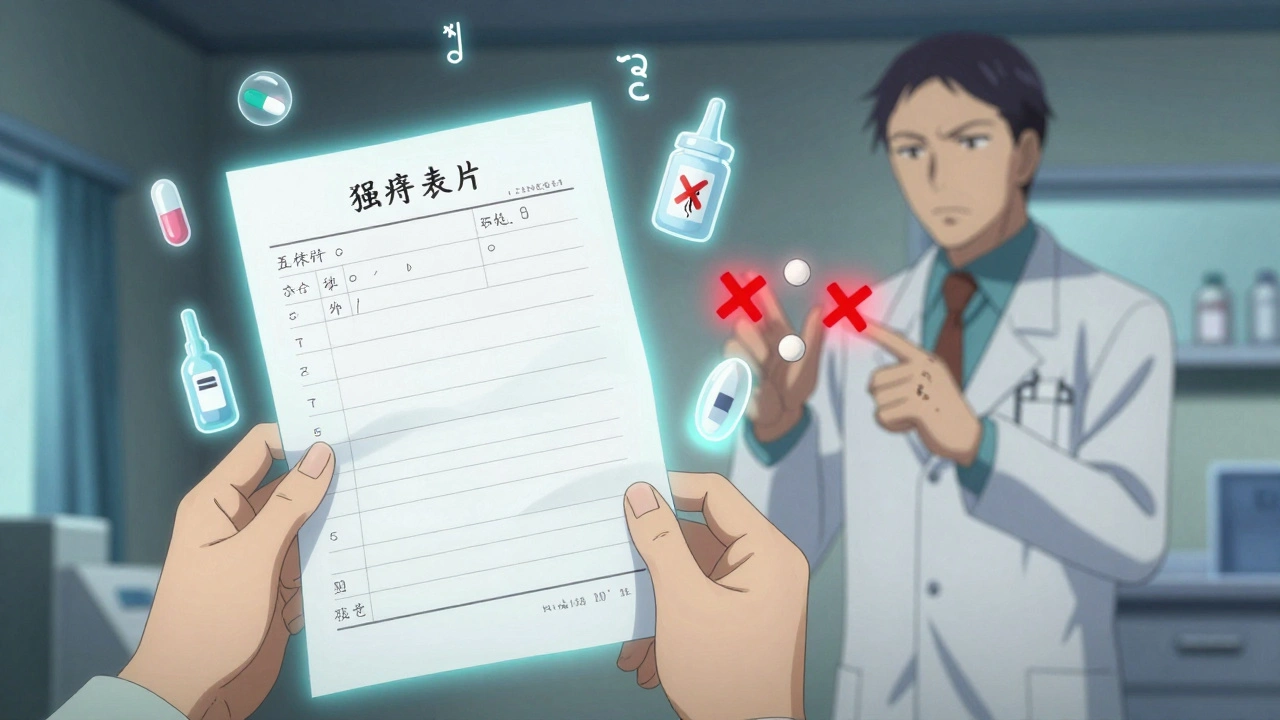
Good discharge planning, a structured process that prepares patients for life after hospitalization. Also known as transition of care, it means knowing exactly what meds to take, when, and why. It means understanding warning signs that mean you need to go back. It means having a follow-up appointment scheduled before you walk out the door. Too many people get a thick stack of papers, a bag of pills, and a vague "call if you feel worse." That’s not care—that’s a gamble. Medication reconciliation, the process of comparing a patient’s current medications with those prescribed at discharge. Also known as med review, it catches errors like duplicate drugs, missing doses, or dangerous interactions. One study found that over 50% of discharge med errors could have been caught with a simple checklist. You don’t need a doctor to do this—you need to ask for it.
And it’s not just about pills. Post-hospital care, the support and services needed after leaving the hospital to prevent readmission. Also known as continuing care, it includes home health visits, physical therapy, dietary help, or even someone to help you get to the bathroom. If you’re older, have multiple conditions, or live alone, this isn’t optional—it’s essential. Many people assume family will step in, but families are often overwhelmed, confused, or live far away. Hospitals are required to assess your needs, but they won’t push unless you do. Ask: "What do I need at home? Who helps me get it? What if I can’t do this alone?"
And don’t forget patient safety. That’s the big one. A wrong dose, a missed allergy, a confusing instruction—any of these can land you right back in the ER. You’re the last line of defense. Write down your meds. Bring a list to every appointment. Know your diagnosis in plain language. If your discharge summary says "follow up with PCP," ask for the name, number, and when. Don’t assume someone else will handle it. The system is full of gaps. You’re the only one who can plug them.
Below, you’ll find real advice from people who’ve been there—how to spot dangerous discharge mistakes, how to get the right meds at the right price, how to avoid being sent home with something that could kill you, and what to do when no one seems to care. These aren’t theory pieces. They’re survival guides written by patients, pharmacists, and nurses who’ve seen what happens when discharge goes wrong—and how to make it right.
How to Reconcile Medications After Hospital Discharge to Avoid Dangerous Interactions
Learn how to prevent dangerous drug interactions after hospital discharge by mastering medication reconciliation-step by step, from admission to follow-up. Know what to ask, what to check, and when to act.