Medication Dysosmia Checker
Check Your Medication Risk
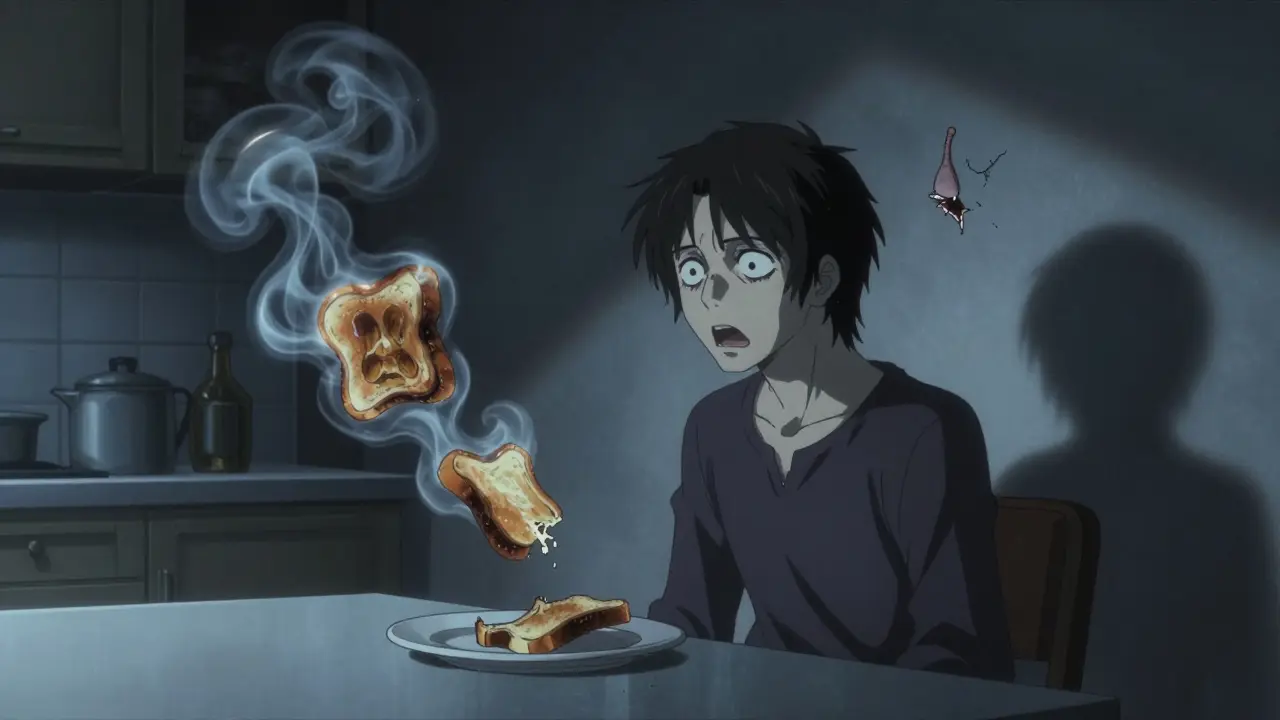
Have you ever taken a medication and suddenly noticed that your favorite food tastes like metal, smoke, or rotten eggs? Or maybe you smell something that isn’t there - like burnt toast or gasoline - when no one else does? You’re not alone. More people than you think experience this, and it’s often linked to the pills they’re taking. This isn’t just a weird quirk. It’s a real, documented side effect called dysosmia.
What Exactly Is Dysosmia?
Dysosmia means your sense of smell is broken - not gone, but twisted. It’s not the same as losing your sense of smell entirely (that’s anosmia). With dysosmia, things you used to smell just fine now smell awful. Coffee might smell like sewage. Bread could smell like burning plastic. And sometimes, you smell something that isn’t there at all. This isn’t in your head. It’s happening in your nose and brain, and it’s being triggered by medications.
This isn’t rare. Over 500 medications are known to cause this. That’s more than half the drugs on the market. And it’s not just about smell - taste gets tangled up too. Since taste relies heavily on smell, when your nose misfires, your whole eating experience falls apart. People report losing their appetite, dropping weight, or even avoiding meals because food tastes unbearable. One study found that 30% of people with medication-induced smell changes lost significant weight because they couldn’t stand what food tasted like.
Which Medications Cause This?
It’s not just one class of drugs. It’s across the board. But some are way more likely to cause trouble than others.
Antibiotics top the list. Fluoroquinolones like levofloxacin and moxifloxacin, and macrolides like azithromycin and clarithromycin, are notorious. These drugs interfere with zinc and magnesium in your nose, which are critical for smell cells to work properly. One study showed people taking levofloxacin were over twice as likely to develop a metallic taste within days. A woman in a 2021 case study lost 8 pounds in three weeks after starting the drug - her food tasted like bile. Even after she stopped taking it, the smell distortion lasted.
Heart medications like midodrine (used for low blood pressure) also show up often. They don’t affect zinc like antibiotics do. Instead, they mess with nerve signals in your nose, making your brain interpret smells incorrectly.
Neurological drugs like carbamazepine (for seizures) and baclofen (for muscle spasms) can cause complete loss of taste alongside smell distortion. One patient reported not being able to taste salt or sugar at all after starting carbamazepine - and the smell of cooked meat became unbearable.
Even IV drugs like lidocaine or iron infusions can cause instant metallic tastes - sometimes within seconds. That’s because they hit your taste receptors directly.

Why Does This Happen?
Your nose doesn’t just detect smells - it has a whole system of sensors, signals, and shut-off switches. Medications interfere with this system in different ways.
- Blocking receptors: Some drugs stick to the smell receptors in your nose and prevent odor molecules from binding. Your brain gets no signal.
- Sticking receptors: Other drugs stop the receptors from turning off. So your nose keeps sending signals even when there’s no smell - that’s why you smell smoke when none is there.
- Disrupting ion channels: Your smell cells use calcium and sodium to send signals. Drugs like fluoroquinolones block these channels, scrambling the message.
- Chelating minerals: Antibiotics bind to zinc and magnesium in your nasal lining. These minerals are needed for smell cells to regenerate. Without them, the cells die off or misfire.
This is why the same drug can cause different symptoms in different people. One person’s nose might get stuck in "on" mode. Another’s might just stop working. It depends on how their body reacts.
How Long Does It Last?
Most cases get better. About 78% of people see improvement within three months of stopping the drug. But 22% don’t. Some symptoms stick around for months - even years.
Reddit threads and patient forums are full of stories. One person described 22 months of food tasting like rotten eggs after taking azithromycin. Another said they couldn’t smell gas leaks - a serious safety risk. The good news? A lot of people do recover. In a 2023 survey of over 400 patients, 65% saw improvement within four weeks of stopping the medication.
But here’s the catch: many doctors don’t ask about smell changes. They check for nausea, dizziness, or headaches - but rarely ask, "Has anything you eat or smell changed?" A 2022 survey found only 37% of primary care doctors routinely ask patients about smell or taste changes. That means a lot of cases go unnoticed - or worse, misdiagnosed as depression, anxiety, or even neurological disease.

What Can You Do?
If you notice smell or taste changes after starting a new medication:
- Don’t panic. It’s likely temporary.
- Track it. Write down what changed, when it started, and what foods smell or taste odd.
- Don’t stop the drug on your own. Some medications - like antibiotics for serious infections or heart drugs - can’t be stopped without medical supervision.
- Talk to your doctor. Ask if the drug is known to cause smell changes. Ask if there’s an alternative.
- Get tested. Specialists can use the University of Pennsylvania Smell Identification Test (UPSIT) to measure your smell function. It’s not perfect, but it helps rule out other causes like sinus infections or neurological issues.
There’s no magic cure. Zinc supplements are often suggested, but they don’t work for everyone. In fact, taking zinc without knowing you’re deficient can cause copper deficiency and make things worse. The same goes for theophylline or magnesium - they only help in specific cases, and only under medical supervision.
One exception? Mirtazapine, an antidepressant sometimes used off-label. In a few case reports, taking 15mg at bedtime cleared up taste distortion within days. But again - this is not a standard treatment. It’s only tried in rare cases.
The Bigger Picture
This isn’t just about food. Smell is tied to safety, memory, emotion, and connection. You can’t smell smoke, gas, spoiled milk, or a burning stove. You lose the scent of rain, coffee, or a loved one’s perfume. People with long-term dysosmia report feeling isolated, anxious, and even depressed.
There’s growing awareness. The FDA now encourages drug makers to include smell and taste changes in clinical trials. The European Medicines Agency plans to require these assessments for antibiotics and heart drugs by 2024. And researchers are testing new drugs that target the exact receptors involved - like TRPM5 channel modulators - which could one day reverse the damage.
For now, the best thing you can do is speak up. If you notice something’s off with your sense of smell or taste after starting a new medication - tell your doctor. Ask if it’s a known side effect. Ask if there’s another option. You’re not imagining it. And you’re not alone.
Can medications cause permanent smell loss?
Yes, in rare cases. While most people recover within weeks or months after stopping the medication, about 22% of cases involve persistent symptoms lasting over a year. This is more common with antibiotics like levofloxacin and azithromycin, and with drugs that damage the olfactory epithelium directly. Permanent loss is uncommon, but it does happen - especially if the condition goes unnoticed for months.
Why don’t doctors talk about this?
Because they’re not trained to. Smell and taste changes aren’t listed as mandatory side effects in most drug labels. Most doctors focus on life-threatening reactions like rashes, swelling, or liver damage. A 2022 survey found only 37% of primary care physicians routinely ask patients about smell changes during medication reviews. It’s an oversight - not intentional neglect.
Is there a test for medication-induced dysosmia?
Yes. The University of Pennsylvania Smell Identification Test (UPSIT) is the gold standard. It’s a 40-item scratch-and-sniff test that measures your ability to identify common odors. It’s not available in every clinic, but otolaryngologists and smell specialists use it to rule out other causes like sinus disease or neurological conditions. It doesn’t prove a drug caused the issue, but it helps confirm the problem is real and measurable.
Can zinc supplements help restore smell?
Only if you’re deficient - and most people aren’t. While zinc plays a role in smell cell regeneration, studies show supplementing zinc doesn’t help people with drug-induced dysosmia unless they have a true deficiency. In fact, too much zinc can cause copper deficiency, which may worsen neurological symptoms. Don’t self-treat with zinc without a blood test and medical advice.
What should I do if I can’t smell smoke or gas?
Install smoke and carbon monoxide detectors in your home - and check them monthly. Relying on your nose for safety is dangerous if you have dysosmia. Consider smart home alerts that detect smoke or gas leaks and send phone notifications. Talk to your doctor about whether your medication should be changed. Never delay replacing a faulty detector.