Rosuvastatin Dose Calculator
Determine Your Safe Starting Dose
This calculator helps determine the appropriate starting dose of rosuvastatin based on your kidney function, age, and ethnicity. Always consult your doctor before making any changes to your medication.
Rosuvastatin is one of the most powerful statins available today. If you’ve been prescribed this medication, you’re likely trying to lower your LDL cholesterol - the kind that clogs arteries and raises heart attack risk. But with great power comes important responsibilities. Rosuvastatin can reduce LDL by up to 63%, but it also carries risks you can’t ignore. Knowing what to monitor isn’t just about following doctor’s orders - it’s about staying safe while getting the full benefit.
Why Rosuvastatin Stands Out
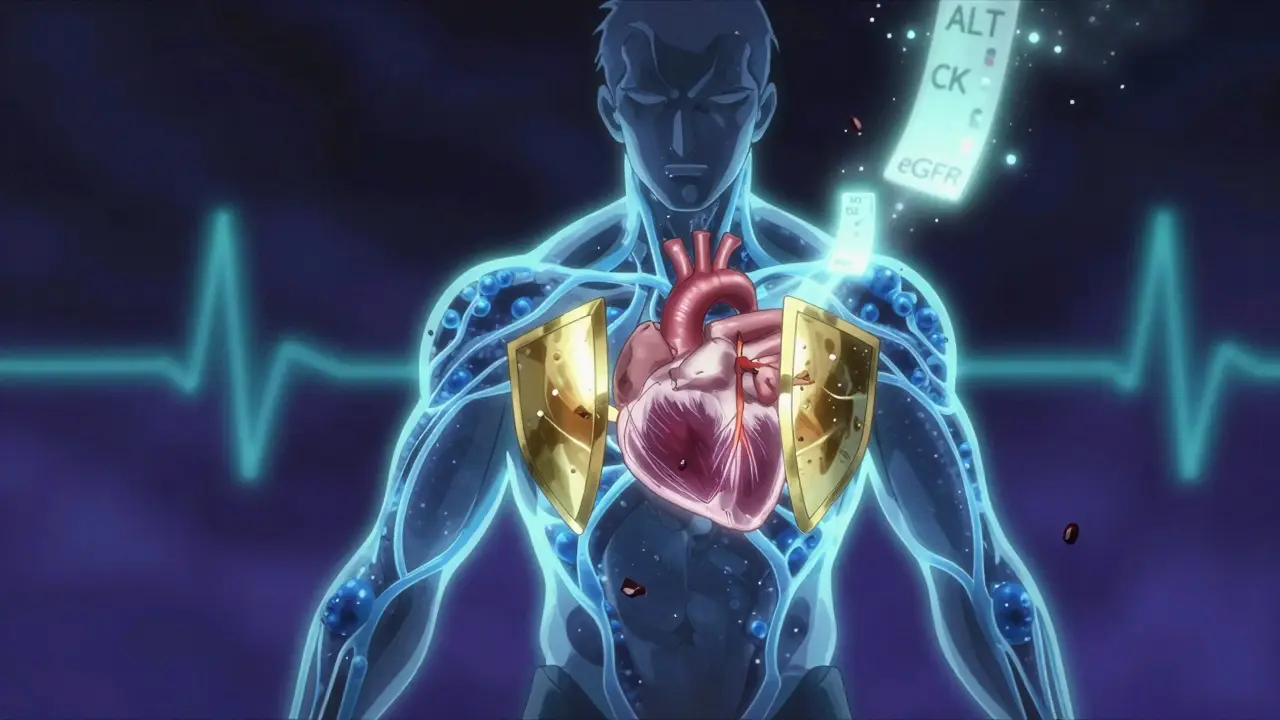
Rosuvastatin, sold under the brand name Crestor, isn’t just another statin. It’s significantly stronger than older options like simvastatin or atorvastatin. At a 20 mg dose, it drops LDL cholesterol by about 55%. Compare that to atorvastatin 20 mg, which lowers it by roughly 40%. That difference matters when you’re trying to hit aggressive targets - especially if you’ve had a heart attack, have diabetes, or carry high genetic risk. Its strength comes from how it works. Rosuvastatin blocks HMG-CoA reductase, the enzyme your liver uses to make cholesterol. But unlike many statins, it doesn’t rely heavily on liver enzymes (CYP3A4) to break down. Only 10% of rosuvastatin is metabolized this way, which means fewer dangerous interactions with other drugs. That’s why it’s often chosen for patients taking multiple medications. It’s also hydrophilic - meaning it doesn’t easily cross into brain tissue. That might explain why some people report fewer brain-related side effects like brain fog compared to lipophilic statins like simvastatin. But this same trait means it’s cleared mostly by the kidneys. And that’s where things get tricky.What You Must Monitor: The Big Five
There are five key things your doctor should check before and during treatment. Ignoring any one of them can lead to serious problems.- Liver enzymes (ALT, AST) - These are measured before you start and again after three months. If they rise above three times the normal level, your doctor may stop the drug. But here’s the twist: routine monthly testing isn’t needed if you feel fine. The FDA updated guidelines in 2012 because most liver issues are silent and rare. Only test if you have symptoms like dark urine, yellowing skin, or unexplained fatigue.
- CK levels (creatine kinase) - This enzyme leaks into the blood when muscle cells break down. You don’t need a blood test unless you feel muscle pain, weakness, or cramps - especially if it’s severe or comes with fever or dark urine. That could mean rhabdomyolysis, a rare but dangerous condition that can damage kidneys. If CK is over 1,000 U/L, you’ll likely need to stop rosuvastatin.
- Estimated GFR (kidney function) - Rosuvastatin is cleared by the kidneys. If your eGFR drops below 60 mL/min/1.73m², you shouldn’t take the 40 mg dose. If it’s below 30, you shouldn’t take it at all. Many people don’t realize their kidneys are slowing down until it’s too late. A simple blood test every year (or more often if you have diabetes or high blood pressure) can catch this early.
- Blood sugar (HbA1c and fasting glucose) - Rosuvastatin slightly increases your risk of developing type 2 diabetes. Studies show it raises HbA1c by 0.1-0.3% and fasting glucose by 5-10 mg/dL. That’s small, but if you’re prediabetic or overweight, it matters. Your doctor should check your HbA1c before starting and again after six months. If it climbs, they might adjust your dose or switch you.
- Protein in urine - This is often overlooked. Rosuvastatin can cause proteinuria - excess protein in urine - especially at 40 mg. It’s usually mild and doesn’t harm kidneys, but if it shows up on a routine urine test, your doctor should reassess your dose. The FDA flagged this in 2016 after finding a 2.3-fold increase in proteinuria at 40 mg vs. 10 mg.
Common Side Effects - And When to Worry
Most people tolerate rosuvastatin well. But side effects happen. About 44% of users report positive results - their cholesterol drops, and they feel better. But 38% report problems, according to user reviews on Drugs.com. The most common complaint? Muscle pain. Around 5-10% of users feel mild aches, especially in the legs or shoulders. This often goes away after a few weeks. But if it’s severe, persistent, or makes it hard to climb stairs or get out of a chair - stop the drug and call your doctor. Don’t wait. Other common issues include:- Headaches - usually mild and temporary
- Nausea or stomach upset - often improves with food
- Memory issues - rare, and usually reversible if you stop the drug
- Increased blood sugar - as mentioned, it’s small but real

Dosing Matters - Less Can Be More
Many people start on 20 mg because it’s labeled as a “high-intensity” dose. But you don’t always need that much. In fact, 10 mg lowers LDL by about 45% - still enough for most people. The 40 mg dose is reserved for those with very high risk and stubborn cholesterol levels. A 2023 study in the Journal of the American College of Cardiology showed that 10 mg of rosuvastatin reduced LDL by 48% in patients with familial hypercholesterolemia - and had far fewer side effects than 20 mg. Many doctors now start at 5 or 10 mg and only increase if needed. If you’re older, have kidney issues, or are Asian (which affects how your body processes the drug), you may need a lower dose. The FDA recommends 5 mg as the starting dose for Asian patients because they tend to have higher blood levels of rosuvastatin.Who Should Avoid Rosuvastatin
Not everyone should take this drug. Avoid it if you:- Have active liver disease
- Are pregnant or breastfeeding
- Have severe kidney disease (eGFR below 30)
- Have had a serious muscle reaction to another statin
- Are taking cyclosporine or gemfibrozil - these drugs can dangerously raise rosuvastatin levels

What to Do If You Experience Side Effects
If you feel muscle pain, don’t just tough it out. Call your doctor. Don’t stop on your own unless symptoms are severe - like dark urine or inability to move your limbs. Your doctor might:- Reduce your dose to 5 or 10 mg
- Switch you to pravastatin or fluvastatin - both are safer for kidneys
- Check for other causes - like thyroid problems or vitamin D deficiency - which can mimic statin side effects
- Test for SLCO1B1 gene variants - some people have a genetic change that makes them more sensitive to rosuvastatin
The Bigger Picture: Benefits vs. Risks
Let’s be clear: rosuvastatin saves lives. The JUPITER trial showed that in people with normal LDL but high inflammation (CRP), rosuvastatin cut heart attacks and strokes by 44%. The METEOR trial found it slowed artery plaque buildup. The American Heart Association says for every 100 people who take a high-intensity statin like rosuvastatin, 1-2 heart attacks are prevented over five years. The risk of serious side effects? Less than 1 in 1,000. As Dr. Paul Ridker, lead researcher of JUPITER, said: “The benefits far outweigh the risks when monitored properly.” You’re not taking this drug to feel perfect. You’re taking it to avoid a heart attack, stroke, or death. That’s the goal. And with smart monitoring, you can get there safely.Final Checklist: What to Do Next
If you’re on rosuvastatin, here’s your simple action plan:- Get baseline blood tests: liver enzymes, kidney function (eGFR), CK, HbA1c
- Report any muscle pain, weakness, or dark urine immediately
- Ask your doctor if you really need 20 mg - could 10 mg work?
- Get kidney and blood sugar checked at least once a year
- Don’t skip follow-ups - even if you feel fine
- Keep a symptom journal - note when pain starts, what you were doing, and if it improves
Can rosuvastatin cause diabetes?
Yes, rosuvastatin slightly increases the risk of developing type 2 diabetes - about 9-12% higher than placebo, based on meta-analyses. This is true for all statins, not just rosuvastatin. The increase in blood sugar is small - typically a 5-10 mg/dL rise in fasting glucose and a 0.1-0.3% rise in HbA1c. For people already at risk (overweight, prediabetic, or with family history), doctors should monitor HbA1c before starting and after six months. The benefit of preventing heart attacks still outweighs this small risk for most patients.
Is muscle pain from rosuvastatin permanent?
No, muscle pain from rosuvastatin is almost always reversible. In most cases, symptoms improve within weeks after stopping or lowering the dose. A 2020 study found that 89% of patients who stopped statins due to muscle pain saw full recovery within six weeks. Rarely, if rhabdomyolysis occurs and isn’t treated quickly, kidney damage can happen - but this is extremely uncommon, affecting fewer than 0.02% of users. If you have muscle pain, don’t panic - but do contact your doctor.
Can I take rosuvastatin with grapefruit juice?
Yes, unlike some other statins like simvastatin or atorvastatin, rosuvastatin is not affected by grapefruit juice. That’s because it doesn’t rely on the CYP3A4 liver enzyme for breakdown, which grapefruit inhibits. You can safely drink grapefruit juice while taking rosuvastatin. This is one reason why rosuvastatin is often preferred for patients who regularly consume grapefruit.
Why is kidney function checked before starting rosuvastatin?
Rosuvastatin is cleared from the body mainly through the kidneys. If your kidney function is poor (eGFR below 60), your body can’t remove the drug as efficiently. This leads to higher levels in your blood, increasing the risk of muscle damage and other side effects. For eGFR between 30-59, the maximum safe dose is 10 mg. Below 30, rosuvastatin is not recommended. Checking kidney function before starting prevents dangerous buildup and ensures the dose is safe for your body.
Are there better alternatives to rosuvastatin?
It depends on your needs. If you need maximum LDL reduction and have healthy kidneys, rosuvastatin is among the best. But if you have kidney disease, liver issues, or had side effects with statins, alternatives exist. Pravastatin and fluvastatin are safer for kidneys and have fewer drug interactions. Atorvastatin is almost as potent and may be better tolerated by some. For people with muscle pain, lower-dose rosuvastatin or switching to ezetimibe (a non-statin cholesterol drug) may be options. Your doctor will choose based on your health, risk level, and tolerance.



Nicole K.
December 29, 2025 AT 16:38This is why people shouldn't be allowed to take statins without a background check. If you're lazy and eat junk, don't blame the medicine when your body rebels. Rosuvastatin isn't the problem - your lifestyle is.
Stop blaming pills and start blaming yourself.
Greg Quinn
December 29, 2025 AT 20:09It's fascinating how we treat medication like a moral test. Rosuvastatin doesn't care if you're 'responsible' or not - it just works. The real question isn't whether you deserve it, but whether the system is set up to help you use it safely.
Maybe we should stop shaming and start supporting.
Lisa Dore
December 29, 2025 AT 22:40I was on 20mg for a year and had zero issues - but I also walked 6 miles a day, ate veggies like they were going out of style, and slept like a baby. It’s not magic, but it works better when you team up with it.
You got this. Small steps matter more than perfection.
Sharleen Luciano
December 30, 2025 AT 07:07Let’s be honest - most people who complain about statin side effects are either hypochondriacs or have never heard of a Mediterranean diet. The fact that you’re reading this means you’re probably overmedicated and undereducated.
Real health isn’t found in a pill bottle - it’s found in discipline, restraint, and the courage to face your own choices.
And yes, grapefruit juice is for amateurs who think flavor trumps function.
Jim Rice
December 30, 2025 AT 10:03Actually, the JUPITER trial was funded by AstraZeneca. You think they’d say anything negative? The real risk is that you’re being sold fear to sell pills.
Statins don’t prevent heart attacks - they prevent lawsuits.
Teresa Rodriguez leon
December 30, 2025 AT 11:57I stopped rosuvastatin because my legs felt like they were made of concrete. I cried for three days. My doctor said I was being dramatic. I felt like I was losing my body. No one gets it.
Why does no one talk about how lonely this feels?
Manan Pandya
January 1, 2026 AT 05:15Excellent breakdown. I appreciate the emphasis on eGFR and proteinuria - many clinicians overlook this. For Indian patients, especially those with metabolic syndrome, starting at 5mg is often sufficient and safer.
Genetic testing for SLCO1B1 is underutilized here, but it’s worth discussing with your pharmacist.
Paige Shipe
January 3, 2026 AT 02:04So let me get this straight - you’re saying if I have high cholesterol and I’m overweight, I should just accept that I’m going to get diabetes because of the medicine? That’s not science. That’s surrender.
And why is everyone so obsessed with 20mg? I’m not a marathon runner, I’m a 45-year-old mom. I need balance, not brute force.
Emma Duquemin
January 4, 2026 AT 05:01OMG I just found out my proteinuria was from rosuvastatin - I thought it was just my period or stress or something??
My doctor was like ‘eh, it happens’ - HELLO? That’s not okay! I’m telling everyone. If you’re on this med, get a urine test. Don’t wait until you’re leaking protein like a sieve.
Also - grapefruit juice is my BFF now. 🍊
Kevin Lopez
January 4, 2026 AT 08:00LDL reduction ≠ clinical benefit. Statin myopathy incidence >10%. NNT 100 for primary prevention. Risk-benefit ratio skewed in low-risk cohorts. Monitor CK, eGFR, HbA1c. Done.
Duncan Careless
January 4, 2026 AT 23:59I’ve been on 10mg for 3 years. My kidneys are fine, my sugar’s steady, and my LDL’s at 72. I didn’t change my diet much - just took it. Sometimes the simplest thing works.
Don’t overthink it. But do listen to your body.
Samar Khan
January 6, 2026 AT 22:35LOL at people who think this is ‘safe’. I had rhabdo at 10mg. Kidneys nearly gave out. Now I’m on ezetimibe and I feel like a new person. Statins are a scam. 💀🩸
Russell Thomas
January 8, 2026 AT 13:34Oh wow, so now we’re giving medical advice based on a Reddit post? Next you’ll tell me to take vitamin C for cancer.
Thanks for the free malpractice lecture, doc.
Fabian Riewe
January 9, 2026 AT 04:01My dad’s 78, has diabetes, and takes 5mg. He’s still hiking. He checks his labs, eats his greens, and doesn’t stress. That’s the secret - not the dose, not the brand. Just show up.
You’re doing better than you think.
Amy Cannon
January 10, 2026 AT 09:52It is of paramount importance to underscore, with the utmost gravity and scholarly rigor, that the pharmacokinetic profile of rosuvastatin - particularly its renal excretion pathway and its relative insensitivity to CYP3A4-mediated metabolism - renders it a uniquely advantageous agent within the statin class, especially in polypharmacy contexts wherein drug-drug interactions constitute a clinically significant concern.
Moreover, one must not overlook the subtle yet statistically significant elevation in glycosylated hemoglobin observed in meta-analyses of randomized controlled trials - a phenomenon which, while modest in magnitude, carries profound implications for the metabolic trajectory of predisposed individuals.
Therefore, it is incumbent upon the prescriber, and indeed the patient, to engage in a dialectical, ongoing dialogue regarding therapeutic goals, risk stratification, and the ethical imperative of informed consent - lest we succumb to the seductive fallacy of pharmacological determinism.