Renal Dosing Calculator
Renal Dosing Calculator
Results
Antibiotic Dosing Recommendations
Based on your calculated CrCl value:
When you have kidney disease, taking the same antibiotic dose as someone with healthy kidneys can be dangerous. Too much drug builds up in your body and can cause seizures, nerve damage, or even death. Too little, and the infection doesn’t get treated-leading to longer hospital stays, worse outcomes, or worse, death. This isn’t speculation. Studies show that inappropriate antibiotic dosing in people with kidney disease increases death risk by up to 27% in pneumonia cases. It’s not a matter of "being careful." It’s a matter of knowing exactly how much to give-and when.
Why Kidneys Matter for Antibiotics
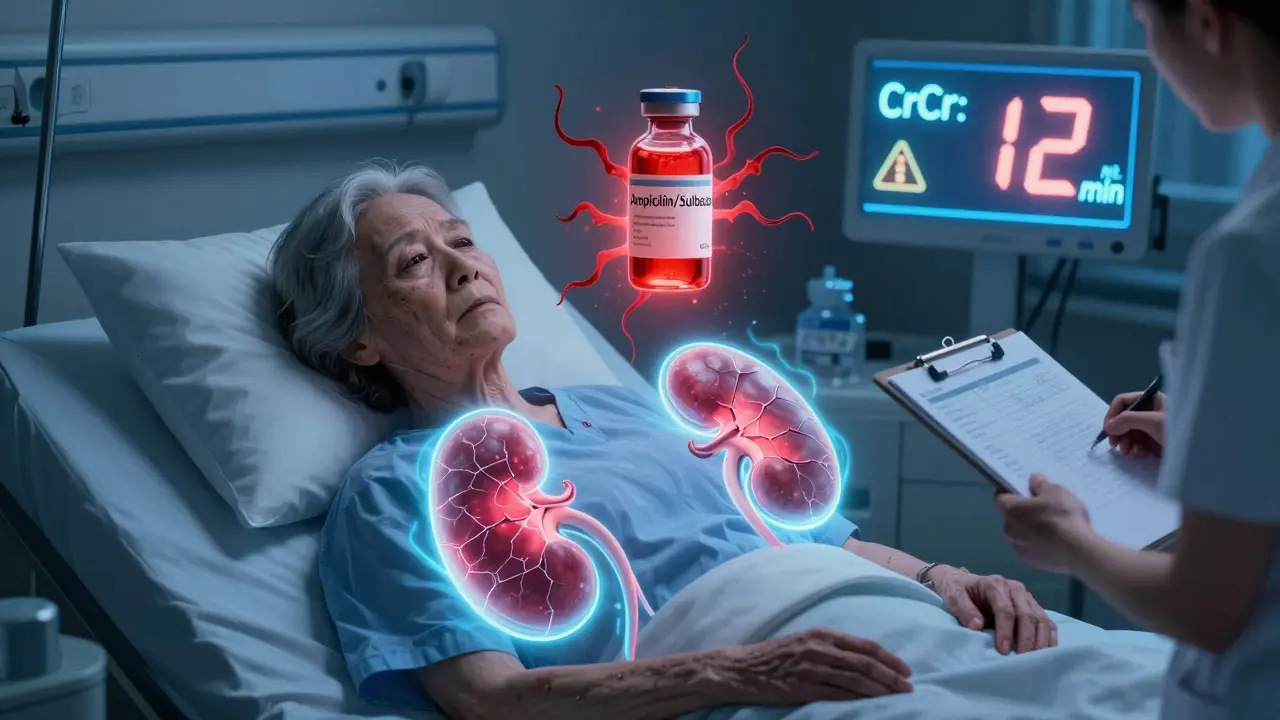
Most antibiotics leave the body through the kidneys. If your kidneys aren’t working well, those drugs don’t get cleared. They pile up. Even if you’re not on dialysis, even if you feel fine, your kidney function might be at 20% or less. That’s enough to turn a safe dose into a toxic one. Take ampicillin/sulbactam. The standard dose is 2 grams every 6 hours. But if your creatinine clearance (CrCl) is below 15 mL/min, that same dose can cause brain toxicity-confusion, seizures, coma. The fix? Cut it to 2 grams every 24 hours. Simple. But only if someone checks your kidney numbers.How We Measure Kidney Function
You’ve probably heard of "creatinine" on a blood test. But creatinine alone doesn’t tell the full story. A 70-year-old woman with a creatinine of 1.2 might have the same kidney function as a 30-year-old man with a creatinine of 0.9. That’s why we use the Cockcroft-Gault equation. It’s old, yes-but it’s still the gold standard. Here’s how it works:- CrCl = [(140 − age) × weight (kg)] / [72 × serum creatinine (mg/dL)]
- Multiply by 0.85 if you’re female
- (140 − 65) = 75
- 75 × 60 = 4500
- 72 × 1.5 = 108
- 4500 / 108 = 41.7
- 41.7 × 0.85 = 35.4 mL/min
What’s Normal? What’s Impaired?
Here’s how kidney function is broken down for dosing:- Normal: CrCl >50 mL/min - standard dose
- Mild: CrCl 31-50 mL/min - reduce dose or extend interval
- Moderate: CrCl 10-30 mL/min - significant reduction
- Severe: CrCl <10 mL/min or on dialysis - very low dose, or only after dialysis
Common Antibiotics and Their Adjustments
Not all antibiotics need changes. Some are mostly cleared by the liver. But many aren’t. Here’s what you need to know:Ampicillin/Sulbactam
- Normal: 1.5-3 g IV every 6 hours
- CrCl 15-29 mL/min: 2 g every 12 hours
- CrCl <15 mL/min: 2 g every 24 hours
Cefazolin
- Normal: 1-2 g IV every 8 hours
- CrCl <10 mL/min: 500 mg-1 g every 12-24 hours
Ceftriaxone
- No adjustment needed at any CrCl level - even in dialysis
Clarithromycin
- Normal: 500 mg every 12 hours
- CrCl <30 mL/min: 500 mg every 24 hours
Ciprofloxacin (oral)
- Normal: 500 mg every 12 hours
- CrCl 10-30 mL/min: 250 mg every 12 hours
- CrCl <10 mL/min: 250 mg every 24 hours
Biggest Mistake: Treating Acute and Chronic Kidney Injury the Same
Here’s where things get messy. Most guidelines are built for patients with long-term kidney disease-people on dialysis, or with stable CKD. But what about someone in the hospital who just had a heart attack, sepsis, or major surgery? Their kidneys might have crashed overnight. That’s acute kidney injury (AKI). And it’s different. In AKI, kidneys can recover fast. Sometimes in 48 hours. But if you reduce the antibiotic dose too early, you risk treatment failure. Studies show underdosing in AKI increases infection failure by 34%. But if you don’t reduce it at all, and their kidneys start bouncing back? Toxicity risk jumps 28%. That’s why some experts say: Don’t reduce antibiotics immediately in AKI unless the patient is truly anuric. Start with the full dose. Recheck CrCl in 24-48 hours. Then adjust.Why Guidelines Don’t Agree
You’d think doctors would have one clear rule. But they don’t. Northwestern Medicine says ceftriaxone needs no dose change at all. UNMC says the same. But for vancomycin? One guideline says load with 25 mg/kg. Another says 20 mg/kg. For piperacillin/tazobactam, UNMC recommends 2 g every 4 hours if CrCl is over 130 mL/min (that’s augmented clearance-seen in young, healthy people with sepsis). Most other guidelines don’t even mention it. A 2023 survey of over 1,200 clinicians found that 63% couldn’t correctly calculate CrCl using Cockcroft-Gault. Nearly a third forgot to use ideal body weight in obese patients. That’s not just a slip-up. That’s a prescription error waiting to happen.How Hospitals Are Fixing This
The good news? Solutions exist.- Electronic alerts: 89% of U.S. hospitals now have EHR systems that flag when a patient’s CrCl is low and suggest dose changes.
- Pharmacist-led programs: Hospitals with dedicated infectious disease pharmacists see 37% fewer antibiotic-related adverse events.
- Standardized protocols: 72% of academic hospitals use KDIGO guidelines as their default.
What You Need to Remember
- Don’t assume normal dosing is safe just because the patient "looks okay."
- Always calculate CrCl using Cockcroft-Gault. Don’t rely on eGFR alone-it’s less accurate for dosing.
- For antibiotics with wide therapeutic windows (like cefazolin), don’t overcorrect. Underdosing can be just as dangerous as overdosing.
- In acute kidney injury, delay dose reduction unless the patient is not making urine at all.
- Always check if a loading dose is needed. For vancomycin, for example, you still need the full loading dose-even if CrCl is low. Just reduce the maintenance dose.
What’s Changing in 2025 and Beyond
The KDIGO guidelines are being updated in 2025 to specifically address acute kidney injury. The FDA now requires new antibiotics to include dosing data for patients with all levels of kidney function. Hospitals are testing AI tools that auto-calculate doses based on real-time labs. Therapeutic drug monitoring-checking blood levels of antibiotics like vancomycin-is expected to jump from 38% to 65% of hospitals by 2027. The message is clear: We’re moving beyond one-size-fits-all dosing. Precision matters. And in kidney disease, precision saves lives.Do all antibiotics need dose adjustments in kidney disease?
No. About 60% of commonly used antibiotics require some form of renal adjustment, but 25% have narrow therapeutic windows where mistakes are dangerous. Others, like ceftriaxone and linezolid, are mostly cleared by the liver and don’t need dose changes even in severe kidney disease.
Can I just use eGFR instead of Cockcroft-Gault?
eGFR is useful for tracking long-term kidney health, but it’s not reliable for antibiotic dosing. The Cockcroft-Gault equation is still the standard because it includes weight and sex-factors that directly affect how drugs are cleared. Using eGFR alone can lead to under- or overdosing.
What if the patient is obese?
Use ideal body weight-not actual weight-in the Cockcroft-Gault equation. Overweight patients often have higher creatinine from muscle mass, which falsely suggests better kidney function. Using actual weight leads to underdosing. For very obese patients, some guidelines suggest using adjusted body weight: IBW + 0.4 × (actual weight − IBW).
Do I need to adjust doses for dialysis patients?
Yes, but it’s more complex. Some drugs are removed during dialysis and need a dose after the session. Others aren’t removed at all and only need a reduced maintenance dose. Always check guidelines for the specific drug and dialysis type (HD, CRRT, etc.). For example, vancomycin is often given after dialysis, while meropenem may need a supplemental dose post-dialysis.
Why do some guidelines say to give a loading dose even with poor kidney function?
For time-dependent antibiotics like vancomycin or piperacillin/tazobactam, reaching the right blood level quickly is critical to kill bacteria. A loading dose gets you there fast. After that, you reduce the maintenance dose to prevent buildup. Skipping the loading dose means the drug takes too long to work-giving the infection time to spread.
Next Steps for Patients and Clinicians
If you’re a patient with kidney disease and you’re prescribed an antibiotic:- Ask: "What’s my creatinine clearance?"
- Ask: "Is this dose adjusted for my kidneys?"
- Ask: "Should I get a blood test in 2-3 days to check if I’m responding?"
- Use Cockcroft-Gault. Always.
- Don’t rely on default EHR doses-check them against current guidelines.
- When in doubt, consult a pharmacist.
- For AKI, hold off on dose reduction for 48 hours unless the patient is anuric.




Jonathan Noe
February 13, 2026 AT 06:51Skilken Awe
February 15, 2026 AT 02:06Jim Johnson
February 16, 2026 AT 17:37Annie Joyce
February 17, 2026 AT 12:23Pat Mun
February 17, 2026 AT 12:41Gloria Ricky
February 17, 2026 AT 17:10Sonja Stoces
February 19, 2026 AT 14:04Kristin Jarecki
February 21, 2026 AT 03:04Luke Trouten
February 22, 2026 AT 05:19Suzette Smith
February 22, 2026 AT 20:52