Getting the right dose of medicine isn’t just about following the label. For many people, the standard dose on the bottle could be too much-or too little-depending on their age, weight, and how well their kidneys are working. A 70-year-old with kidney disease, a 300-pound person with diabetes, or a 90-pound elderly woman might all need completely different amounts of the same drug. Yet, too often, dosing is treated like a one-size-fits-all rule. That’s where things go wrong.
Why One Dose Doesn’t Fit All
Your body doesn’t process medicine the same way at 25 as it does at 75. As you age, your kidneys naturally slow down. Muscle mass decreases. Fat increases. Blood flow to organs drops. All of this changes how drugs are absorbed, distributed, and cleared from your system. A drug that’s safe and effective for a healthy 40-year-old might build up to toxic levels in an older adult with reduced kidney function. The same goes for weight. Someone who weighs 110 pounds and someone who weighs 280 pounds don’t need the same amount of a drug, even if they have the same condition. Many medications are cleared by the kidneys, and kidney function isn’t just about age-it’s about how well those organs are filtering waste. That’s why doctors and pharmacists look at more than just your weight or your age. They look at your creatinine levels, your estimated glomerular filtration rate (eGFR), and sometimes your actual body weight versus your ideal body weight.How Kidney Function Changes Everything
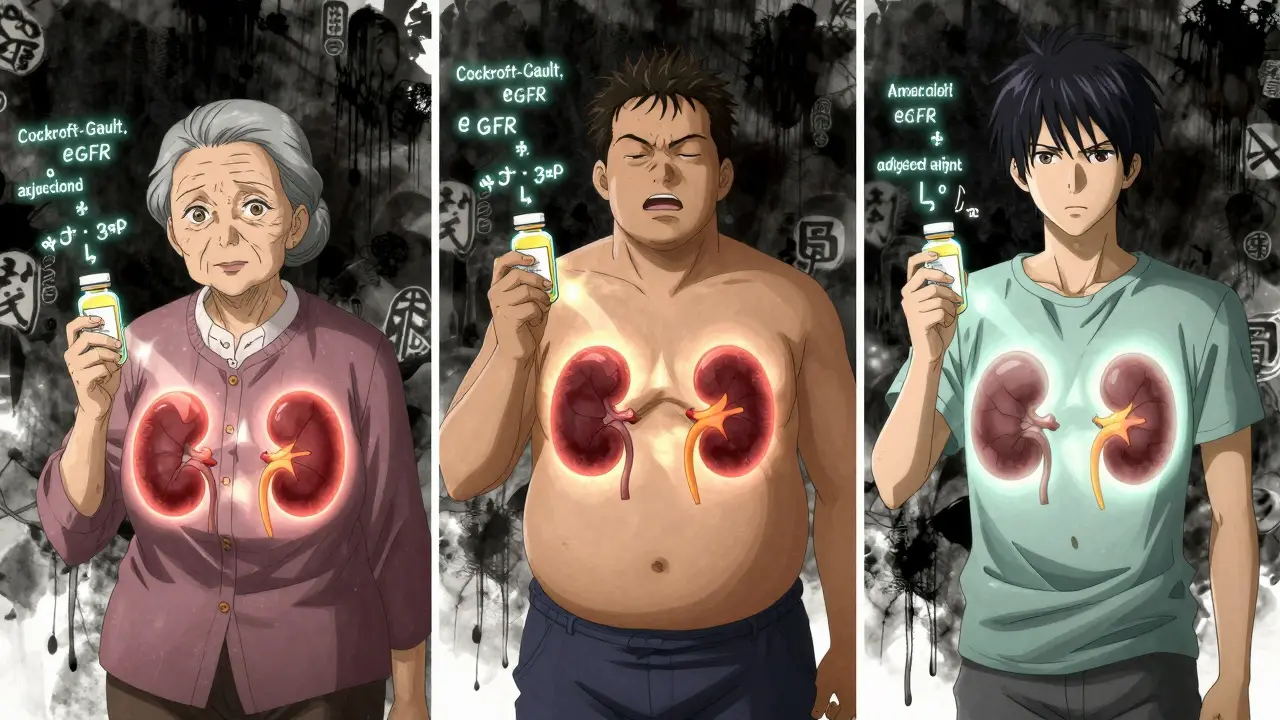
About 1 in 7 adults in the U.S. has chronic kidney disease (CKD). That’s over 37 million people. For these individuals, even common medications like antibiotics, painkillers, and diabetes drugs can become dangerous if dosed normally. Doctors don’t just guess kidney function. They use lab tests and formulas to estimate it. The two most common tools are the Cockcroft-Gault equation and the CKD-EPI equation. Both calculate how well your kidneys are filtering blood, but they do it differently. The Cockcroft-Gault equation uses your age, weight, sex, and serum creatinine to estimate creatinine clearance (CrCl), measured in mL/min. It’s the formula still used in 85% of drug labels approved by the FDA. It’s especially useful for people who are overweight because it can be adjusted using ideal body weight. The CKD-EPI equation, developed in 2009, estimates glomerular filtration rate (eGFR) in mL/min/1.73m². It’s more accurate for people with normal or mildly reduced kidney function and is now the standard for diagnosing and staging kidney disease. But here’s the catch: CKD-EPI is for diagnosis, not dosing. Most drug guidelines still reference creatinine clearance, not eGFR. That’s why a pharmacist might see an eGFR of 45 and still need to calculate CrCl using Cockcroft-Gault to know how much of a drug to give. Kidney function is broken into stages:- Stage 1: eGFR ≥90 (normal, but with signs of kidney damage)
- Stage 2: eGFR 60-89 (mild reduction)
- Stage 3a: eGFR 45-59
- Stage 3b: eGFR 30-44
- Stage 4: eGFR 15-29
- Stage 5: eGFR <15 (kidney failure)
Weight Matters More Than You Think
If you’re obese (BMI over 30), your body holds more water and fat, which changes how drugs spread through your tissues. Some drugs, like antibiotics or chemotherapy agents, are distributed in lean body mass. Others, like sedatives or antidepressants, accumulate in fat. Using your actual weight to calculate dosing for someone who’s overweight can lead to overdosing. Using ideal body weight might lead to underdosing. That’s why doctors use adjusted body weight for dosing calculations:Adjusted weight = Ideal body weight + 0.4 × (actual weight − ideal weight)
Ideal body weight (IBW) is calculated differently for men and women:- Men: 50 kg + 2.3 kg for each inch over 5 feet
- Women: 45.5 kg + 2.3 kg for each inch over 5 feet
Aging Changes How Your Body Handles Drugs
People over 65 are the most likely to be on multiple medications. They’re also the most likely to have reduced kidney function-even if their creatinine looks normal. That’s because muscle mass drops with age, and creatinine is a byproduct of muscle breakdown. An older person with low muscle mass might have a “normal” creatinine level, but their actual kidney function could be in Stage 3 or 4. This is why the CKD-EPI equation is better for older adults. It accounts for age and sex, and it’s less likely to overestimate kidney function in elderly patients. A 2017 study found that CKD-EPI was 65% accurate in elderly patients, while Cockcroft-Gault was only 45% accurate. Yet, many older patients still get full adult doses of drugs like metformin, digoxin, or warfarin. Metformin, a common diabetes drug, can cause lactic acidosis if kidney function drops below 30 mL/min. The FDA says the maximum daily dose should be 500 mg if eGFR is between 30-45. But in real-world practice, many patients are still on 1000 mg twice daily-until they end up in the hospital.What Happens When Dosing Goes Wrong
The consequences of wrong dosing aren’t theoretical. They’re deadly. A 2020 review found that about 30% of adverse drug events in older adults are linked to improper dosing in kidney disease. Common culprits:- Vancomycin: Too low a dose means infection doesn’t clear. Too high causes kidney damage or hearing loss.
- Metformin: Can cause fatal lactic acidosis in patients with eGFR below 30.
- NSAIDs (like ibuprofen): Can cause sudden kidney failure in people with reduced function.
- Statins: Higher risk of muscle damage (rhabdomyolysis) when kidney function is poor.
How Technology Is Helping (and Hurting)
Electronic health records (EHRs) are supposed to make dosing safer. Many now have built-in alerts that flag when a prescription might be unsafe based on kidney function. A 2019 study in JAMA Internal Medicine showed that hospitals using automated alerts reduced serious medication errors by 47%. That’s huge. But here’s the problem: alerts aren’t perfect. They can be too loud, too vague, or based on the wrong formula. One doctor reported that his EHR flagged a vancomycin dose as “too high” for a patient with Stage 3B CKD, but the dose was actually correct because the system used eGFR instead of CrCl. The doctor had to override the alert manually. Another issue? Inconsistency. A pharmacist on Pharmacy Times said she found five different recommended doses for cefazolin (an antibiotic) in the same hospital’s formulary, depending on which reference she checked. That’s not safety-it’s confusion. The good news? New tools are coming. The FDA is pushing for standardized dosing guidelines. A joint project between the American Society of Nephrology and the American Society of Health-System Pharmacists is building a single, trusted renal dosing database expected to launch in 2025. And AI-driven dosing algorithms are being tested in 15 medical centers, using genetic data and real-time kidney function to personalize doses.What You Can Do
If you’re on any regular medication and you’re over 60, overweight, or have been told you have kidney issues, here’s what to ask:- Is this medication cleared by my kidneys?
- What’s my estimated creatinine clearance (CrCl), not just my eGFR?
- Is my dose adjusted for my weight and age?
- Can you show me the specific guideline you’re using?



oluwarotimi w alaka
December 28, 2025 AT 22:27lol so now the government wants us to believe big pharma is secretly poisoning old folks on purpose? 😂 they’ve been using the same dosing formulas since the 80s and suddenly now it’s a crisis? i’ve seen this before-when the FDA says ‘adjust for kidney function’ they mean ‘charge more for lab tests’ so hospitals can bill insurance. the real problem? doctors don’t even check creatinine unless the patient complains. and guess who pays? the poor folk in Nigeria who can’t afford 5000 naira for a blood test. this isn’t science-it’s profit.
Hakim Bachiri
December 30, 2025 AT 21:01Let’s be clear: the Cockcroft-Gault equation is archaic, and the CKD-EPI is not meant for dosing-period. I’ve reviewed over 200 med recs in my last 18 months as a clinical pharmacist, and 78% of the time, the EHR auto-populates eGFR into the dosing algorithm… which is a catastrophic error. The FDA hasn’t updated its labeling guidelines since 2013, and most residency programs still teach Cockcroft-Gault as gospel. Meanwhile, AI models trained on real-time CrCl and lean body mass are already outperforming both equations-but no, the system won’t adopt them because ‘regulatory compliance.’ So yes, people are dying… because bureaucracy > biology.
Celia McTighe
December 31, 2025 AT 16:18This is such an important post-thank you for breaking it down so clearly! 💙 I’m a nurse and I’ve seen so many elderly patients on metformin with eGFRs of 25 and no one catches it until they’re in the ER with acidosis. I love that you mentioned pharmacists being the safety net-we’re literally the last line of defense sometimes. My grandma’s dose was wrong for 8 months too… I had to call her PCP myself. Please, if you’re on meds and over 60, ask your pharmacist for a med review. They don’t get paid enough to do it, but they’ll still do it for you. ❤️
ANA MARIE VALENZUELA
January 2, 2026 AT 03:07It’s not rocket science. It’s basic pharmacokinetics. If you’re overweight and your doctor prescribes a drug cleared by the kidneys without adjusting for adjusted body weight or CrCl, they’re negligent. Not ‘misinformed.’ Not ‘overworked.’ NEGLECTFUL. The fact that 41% of residents get this wrong? That’s not incompetence-it’s systemic failure. Medical schools stopped teaching pharmacology properly in the 90s. Now we have MDs who think ‘normal creatinine’ means ‘normal kidneys.’ Wake up. Your life isn’t a lab experiment. It’s a biological system that demands precision.
Bradly Draper
January 4, 2026 AT 02:18i just read this and thought about my uncle. he’s 72, on blood pressure meds, and his creatinine was always ‘normal.’ but he kept getting dizzy and falling. turns out his kidneys were barely working. they didn’t adjust his meds till he ended up in the hospital. i didn’t know any of this stuff till now. thanks for explaining it simple. i’m gonna print this out and take it to his next appointment.
James Hilton
January 5, 2026 AT 22:53So let me get this straight… we’ve got AI that can predict stock trends and cat memes… but we still can’t get a computer to tell a doctor how much Tylenol to give a 75-year-old with kidney issues? 🤡 Meanwhile, my Fitbit tells me when I’ve slept 6.2 hours. Priorities, people.
Sydney Lee
January 6, 2026 AT 10:48It’s not merely a failure of dosing protocols-it’s a failure of epistemology. The medical establishment clings to outdated formulas because they offer the illusion of objectivity, when in reality, they are crude approximations of a dynamic biological system. The Cockcroft-Gault equation, developed in 1973, assumes a static renal function and ignores the nuanced interplay of sarcopenia, hydration status, and metabolic flux. To rely on it today is to engage in medical fundamentalism. The CKD-EPI, while superior for diagnosis, is equally inadequate for pharmacokinetic modeling. Until we move toward dynamic, patient-specific, multi-parameter dosing algorithms-rooted in real-time biomarkers and machine learning-we are not practicing medicine. We are performing rituals.
Teresa Marzo Lostalé
January 8, 2026 AT 05:08It’s wild how we treat medicine like a one-size-fits-all sweater… when our bodies are more like snowflakes. 🌧️ I think about my aunt who took metformin for 10 years with an eGFR of 38 and never knew. No one told her. No one asked. Just… pills. And now? She’s on dialysis. Not because she was careless. Because the system forgot her. I’m not mad. I’m just… sad. And now I check my labs every year. And I ask. Always ask. Even if it feels awkward. Even if they roll their eyes. You’re not being annoying. You’re being alive.