Every time you write a prescription, you’re not just choosing a drug-you’re choosing a cost. And if that cost isn’t covered, your patient might skip the medication, split pills, or just go without. That’s not hypothetical. In 2024, nearly 1 in 5 Medicare beneficiaries skipped a prescribed drug because of cost. The key to avoiding this? Checking the formulary before you hit send.
What Exactly Is a Formulary?
A formulary, also called a Preferred Drug List (PDL), is the official list of medications your patient’s insurance plan covers. It’s not random. Every drug on it has been reviewed by a committee of doctors and pharmacists who weigh clinical evidence, safety, and price. The goal? To make sure patients get effective treatment without unnecessary spending. These lists aren’t static. They change. Medicare Part D plans update theirs quarterly-January, April, July, October-and can make mid-year changes with 60 days’ notice. A drug that was Tier 1 last month could be Tier 4 next month. If you’re prescribing Januvia, for example, one plan might list it as preferred (Tier 3), another as non-preferred (Tier 4), and a third might require step therapy first. You can’t assume. You have to check.How Formularies Are Structured (The Tier System)
Most formularies use a tier system. The lower the tier, the less the patient pays. Here’s how it typically breaks down in Medicare Part D plans:- Tier 1: Preferred generics-usually $1 to $5 per prescription. Think metformin, lisinopril, atorvastatin.
- Tier 2: Other generics-slightly higher cost, maybe $10-$15.
- Tier 3: Preferred brand-name drugs-often $30-$50. These are drugs with proven effectiveness and good value.
- Tier 4: Non-preferred brands-$50 to $100+. These are often newer or more expensive drugs with little cost advantage.
- Tier 5: Specialty drugs-anything over $950/month. These require coinsurance (e.g., 33% of cost) and often prior authorization.
What Those Letters Mean: PA, ST, QL
Don’t just look at the tier. Look at the symbols next to the drug:- PA (Prior Authorization): You need to call or submit paperwork before the plan will cover it. This can take 24 to 72 hours. For cancer drugs, delays of over 48 hours happen in 32% of cases.
- ST (Step Therapy): The patient must try and fail on a cheaper drug first. For example, you want to start a patient on Ozempic, but the plan requires them to try metformin and then sitagliptin first.
- QL (Quantity Limit): You can only prescribe a certain amount per month. A 90-day supply might be blocked unless you justify it.

Where to Check Formularies (And How to Do It Fast)
You have three main ways to check:- Insurer’s website: Most major insurers-Aetna, UnitedHealthcare, Humana-have a drug search tool. You enter the drug name, the patient’s plan name, and sometimes their zip code. Aetna’s tool was rated “very helpful” by 74% of providers in a 2024 survey.
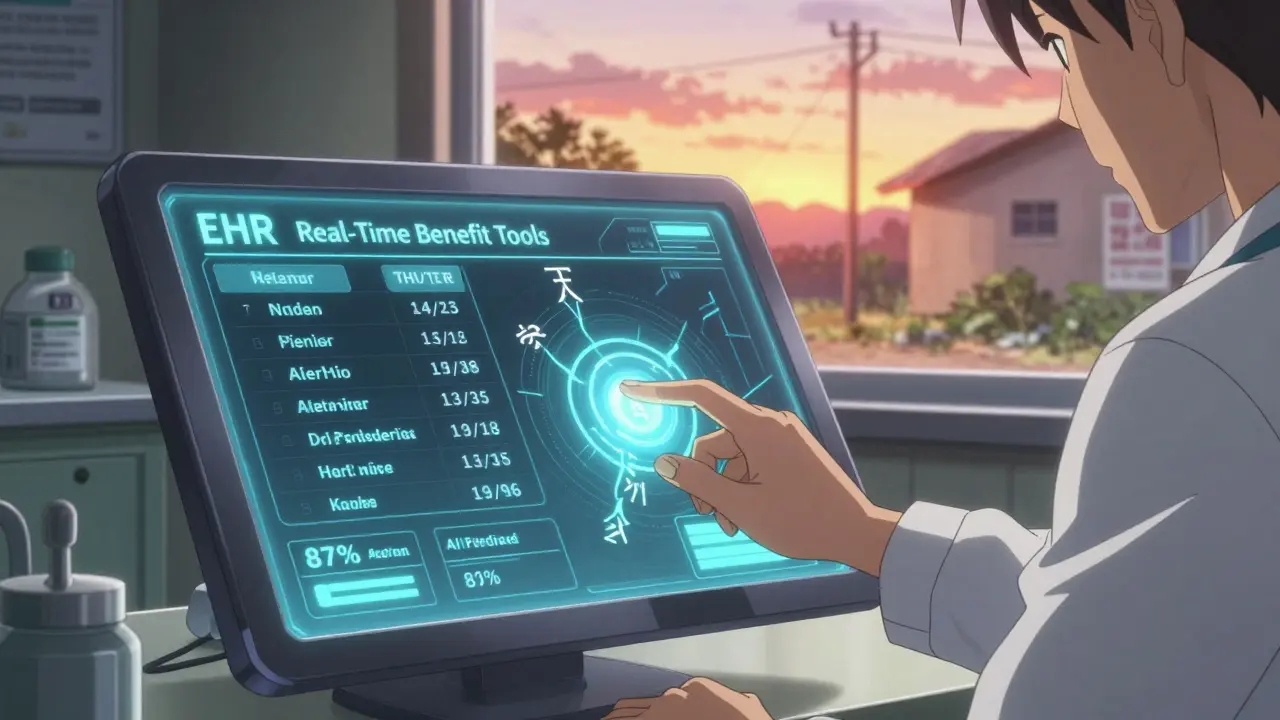
- EHR-integrated tools: If your clinic uses Epic, Cerner, or another major system, check if they’ve enabled the Formulary Check module. Northwestern Medicine cut prescription abandonment by 42% after implementing this in 2023.
- CMS Plan Finder: For Medicare patients, this free tool covers 99.8% of Part D plans. You can search by drug, compare plans, and see tier status and restrictions.
Differences Between Medicare, Medicaid, and Commercial Plans
Not all formularies are created equal:- Medicare Part D: Always uses a five-tier system. Must cover at least two drugs per therapeutic category. Must offer exceptions and appeals.
- Medicaid: Varies by state. 42 states use closed formularies-meaning if a drug isn’t on the list, you need prior authorization just to request it. Minnesota, for example, has a single PDL for all Medicaid members.
- Commercial plans: Often use four tiers. Some don’t require prior authorization for brand drugs. Others have stricter quantity limits. UnitedHealthcare’s 2024 commercial formulary, for instance, doesn’t have a separate specialty tier like Medicare does.
What’s Changing in 2025 and Beyond
The Inflation Reduction Act’s $2,000 annual cap on out-of-pocket drug costs for Medicare starts in 2025. That’s already reshaping formularies. In 2025, 73% of Medicare Part D plans are moving more drugs to lower tiers to keep patients under the cap. Also, by January 1, 2026, all Medicare Part D plans must use Real-Time Benefit Tools (RTBT). That means when you type a drug into your EHR, the system will instantly show you the patient’s cost, tier, and any restrictions-no more logging into separate portals. Some health systems are even testing AI tools. Epic’s FormularyAI, launched in August 2024, predicts whether a prior authorization will be approved based on 10 million historical decisions-with 87% accuracy. It’s not perfect, but it cuts guesswork.Why This Isn’t Optional
A 2023 Sermo survey found that 68% of physicians spend 10 to 20 minutes per patient just verifying coverage. Primary care doctors spend nearly 19 minutes. That’s not administrative busywork-it’s part of prescribing. And the stakes are high. In 2024, 34% of physicians reported that prior authorization delays led to serious adverse events. A patient with diabetes who can’t get their insulin on time? A heart patient whose beta-blocker is denied? These aren’t abstract risks. They’re preventable. You don’t need to be a pharmacy expert. But you do need to treat formulary checks like you treat allergies or drug interactions. It’s part of the prescription.What You Can Do Today
Here’s your action plan:- Identify your top 10 most-prescribed drugs. Check their tier and restrictions on the top three insurers in your area.
- Bookmark the formulary pages. Save direct links to Aetna, UnitedHealthcare, and Medicare Plan Finder.
- Set quarterly reminders. Formularies change. Mark your calendar for January 1, April 1, July 1, and October 1.
- Ask your EHR vendor. Do you have a formulary checker? If not, push for it.
- Train your staff. Have a medical assistant run a quick formulary check before the patient sees you.
What’s the difference between a formulary and a preferred drug list?
They’re the same thing. "Formulary" is the industry term used by insurers and pharmacy benefit managers. "Preferred Drug List" (PDL) is often used by Medicaid programs and government agencies. Both refer to the list of drugs covered by a health plan, organized by cost tiers and usage rules.
Can I prescribe a drug that’s not on the formulary?
Yes, but the patient will likely pay full price unless you request an exception. For Medicare Part D, you can submit a prior authorization request with clinical justification. The insurer must respond within 72 hours (or 24 hours for urgent cases). For Medicaid, it’s harder-many states have closed formularies, meaning non-listed drugs are rarely covered without a complex appeal.
How often do formularies change?
Medicare Part D plans update their formularies quarterly-in January, April, July, and October. They can also make mid-year changes, but they must notify patients and providers 60 days in advance. Commercial insurers vary, but most update at least once a year. Always check before prescribing, even if you prescribed the same drug last month.
Why do two plans cover the same drug at different tiers?
Each insurer negotiates separately with drug manufacturers. One plan might get a better rebate on a brand-name drug, so they put it in Tier 3. Another plan might not have that deal, so they put it in Tier 4. It’s not about clinical value-it’s about price negotiations. That’s why checking the specific plan matters.
Is there a free tool to check Medicare formularies?
Yes. The Medicare Plan Finder on Medicare.gov is free, official, and covers nearly all Part D plans. You can search by drug name, compare multiple plans side-by-side, and see exact costs, tiers, and restrictions. It’s the most reliable source for Medicare patients.
What should I do if a patient can’t afford their prescribed drug?
First, check if there’s a lower-tier alternative on the formulary. If not, submit a prior authorization request with clinical justification. Many insurers have patient assistance programs-ask the pharmacy or call the insurer’s provider line. For Medicare patients, the $2,000 out-of-pocket cap in 2025 will help, but until then, don’t assume cost isn’t a barrier. Always ask: "Can you afford this?"




Jarrod Flesch
January 20, 2026 AT 02:50Been using Epic's formulary checker for a year now-game changer. Used to spend 15 mins per script just calling pharmacies. Now it pops up before I even finish typing. My patients notice. They don't get dropped mid-prescription anymore. 🙌
michelle Brownsea
January 21, 2026 AT 06:36Let me be perfectly clear: if you're not checking formularies before prescribing, you're not just being negligent-you're participating in systemic cruelty. Patients aren't 'inconvenienced'-they're being forced into medical rationing because you refuse to do your job. The fact that this even needs to be said is horrifying.
Gerard Jordan
January 23, 2026 AT 04:41Love this thread. Seriously. I'm a doc in a rural town in Mississippi, and we still print out formulary sheets because the internet here is slower than my grandma’s dial-up. 😅 But we keep them taped to the wall next to the fax machine. One time, a patient cried because she finally got her insulin-no prior auth, Tier 1. That’s why we do this.
Sangeeta Isaac
January 23, 2026 AT 15:49So you're telling me I gotta memorize 5 different rulebooks just to give someone a pill? And the system calls this 'healthcare'? 🤡 I'm pretty sure my cat could do a better job than these insurance algorithms. Also, why does 'Tier 5' sound like a secret society for rich pharma CEOs?
Melanie Pearson
January 25, 2026 AT 00:01It is an incontrovertible fact that the American healthcare system is structurally compromised by the commodification of pharmaceutical access. The tiered formulary system is not a clinical tool-it is a mechanism of economic coercion disguised as fiscal responsibility. The fact that physicians are expected to navigate this labyrinth without institutional support constitutes a violation of medical ethics.
Stephen Rock
January 25, 2026 AT 03:11lol why do we still care about formularies? Just write the script. If they can't afford it, they're not your problem. Your job is to diagnose, not be a pharmacy clerk. Also, Medicare's $2k cap? Cool. Now I can prescribe whatever I want and let the system handle it. Win-win.
Andrew Rinaldi
January 25, 2026 AT 04:10I get why some of you are frustrated. But I think we’re missing the bigger picture. This isn’t about blaming doctors or insurers-it’s about fixing a broken system. The fact that we’re even having this conversation means we’re starting to care. And that’s the first step. Maybe EHR integration is the bridge we need.
Roisin Kelly
January 26, 2026 AT 20:53Anyone else think this whole formulary thing is just a big lie to make people think they have 'choice'? I checked my plan’s formulary last month. Then I called them. They told me the website was 'out of date.' So what’s the point? They don’t even know their own rules. This is all just theater.
Ashok Sakra
January 28, 2026 AT 01:35My cousin in India, he get medicine for $1. Here, same pill cost $80. Why? Because America. Just say it. America bad. People die. Not because sick. Because money.
Uju Megafu
January 30, 2026 AT 01:29Y’all act like this is new. In Nigeria, we’ve been doing formulary checks since the 90s-except we don’t have EHRs. We have WhatsApp groups with pharmacists. One nurse sent me a photo of a prescription with a red stamp: ‘NOT COVERED.’ We took it to the clinic. They cried. We changed the script. That’s how we survive. You guys have tech. Use it.
lokesh prasanth
January 31, 2026 AT 14:37formularies are just a way for big pharma to control what docs prescribe. they pay insurers to put their drugs on tier 3. the science? irrelevant. just look at the rebate numbers.
Kelly McRainey Moore
February 1, 2026 AT 16:01My PA now checks formularies before I even see the patient. Saved me 20 hours a week and stopped three ER visits last month. Seriously, if your clinic doesn’t have this setup, just… ask. Or hire someone who will. It’s not hard.