When you can hear people talking but everything sounds muffled-like they’re speaking through a wall-it’s not just your ears being lazy. It could be conductive hearing loss, a common but often misunderstood issue where sound gets stuck in the outer or middle ear before it reaches the inner ear. Unlike sensorineural hearing loss, which involves nerve damage, conductive hearing loss is often fixable. And in many cases, surgery can restore hearing completely.
What Exactly Is Conductive Hearing Loss?
Conductive hearing loss happens when sound waves can’t move freely through the ear canal, eardrum, or middle ear bones (ossicles). It’s not that your inner ear is broken-it’s that the path to it is blocked or damaged. You might struggle to hear whispers, turn up the TV too loud, or feel like your own voice sounds hollow. This isn’t just an annoyance; it can affect learning in kids, social confidence in adults, and even safety-like not hearing a car horn or a smoke alarm.
Unlike sudden sensorineural hearing loss, which is a medical emergency, conductive loss often develops slowly. But if it shows up suddenly-like after a head injury or loud explosion-it needs immediate attention. The key sign? An air-bone gap. That’s when air-conducted sound (through the ear canal) is weaker than bone-conducted sound (through the skull). Audiologists measure this with specialized tests, not the basic screenings you get at pharmacies or big-box stores.
Common Middle Ear Causes
There are several specific middle ear problems that cause this type of hearing loss. The most common in children is otitis media with effusion-also called glue ear. It’s when fluid builds up behind the eardrum after an infection clears. About 80% of kids have at least one episode by age 3. In many cases, it goes away on its own. But if it sticks around for months, it can delay speech development.
In adults, otosclerosis is a major cause. It’s a genetic condition where the stapes bone-the smallest bone in the body-fuses to the inner ear wall and stops vibrating. You might not notice it at first, but over time, hearing gets worse, especially for low-pitched sounds. It often starts in your 20s or 30s and gets worse with age.
Cholesteatomas are more serious. These aren’t tumors-they’re abnormal skin cysts that grow in the middle ear. They can erode bone, damage the inner ear, and even cause facial paralysis if left untreated. They need surgery, no matter how small they seem. A perforated eardrum is another common culprit, especially after ear infections, trauma, or sudden pressure changes (like scuba diving or flying with a cold). About 15-20% of adult conductive hearing loss cases come from this.
Then there’s aural atresia-a birth defect where the ear canal doesn’t form properly. It affects about 1 in 10,000 babies and often comes with underdeveloped middle ear structures. These kids usually need multiple surgeries to create a working canal and restore hearing.
How Is It Diagnosed?
You can’t diagnose this yourself. A basic hearing test at a drugstore won’t cut it. You need an audiologist who knows how to interpret air and bone conduction results. They’ll also use a tympanometer to check how well your eardrum moves. A flat line on the graph (Type B tympanogram) usually means fluid is trapped behind the eardrum.
If the problem looks structural, you’ll likely get a high-resolution CT scan of your temporal bone. It shows the exact shape of the ossicles, eardrum, and ear canal. These scans cost $800-$1,200 out-of-pocket in the U.S., but they’re essential before surgery. Without them, a surgeon can’t plan the right approach.
The whole diagnostic process takes 2-4 weeks. Doctors don’t rush into surgery. If you’ve had fluid for less than three months, they’ll often wait. For kids, 65% of cases clear up without surgery. But if hearing loss is over 25-30 dB and hasn’t improved after 3-4 months, it’s time to consider options.
Surgical Options That Work
Once the cause is clear, surgery becomes the main path forward. Here’s what’s actually done in real clinics today.
Tympanoplasty is the go-to for eardrum perforations. Surgeons use a graft-often taken from your own tissue, like the temporalis fascia-to patch the hole. Success rates? 85-95% for small tears, 70-85% for larger ones. Recovery takes 6-8 weeks. You can’t get water in your ear, fly, or lift heavy things during that time.
Stapedectomy or stapedotomy treats otosclerosis. The fixed stapes bone is either partially removed (stapedotomy) or replaced with a tiny piston-like prosthesis. Modern laser-assisted techniques have cut complication rates from 15% down to under 2%. After surgery, 80-90% of patients close their air-bone gap to within 10 dB-meaning they hear almost normally again. Many report hearing whispers for the first time in years.
Myringotomy with tubes is the most common pediatric surgery in the U.S., with over 667,000 procedures done each year. A tiny tube is inserted through the eardrum to drain fluid and let air in. Most kids stop getting ear infections within weeks. Around 75% of cases resolve within three months. Some parents report ongoing drainage, but that’s usually manageable with ear drops.
Canalplasty rebuilds the ear canal in babies born with aural atresia. It’s complex-often requiring multiple surgeries-and outcomes vary. About 60-70% achieve functional hearing, but it’s not perfect. Some still need bone-conduction devices later.
Cholesteatoma removal is non-negotiable. The goal isn’t just hearing-it’s stopping destruction. Surgeons remove the cyst and reconstruct damaged parts. Recovery is longer than other procedures-many patients need 4-6 weeks before returning to normal. Some report changes in how sounds feel afterward, even if volume improves.
What to Expect After Surgery
Surgery isn’t a magic fix. Recovery is slow. You’ll have follow-up visits to check healing, remove packing, and test hearing. Most people notice improvement within weeks, but full results take 3-6 months.
Side effects are rare but real. Temporary dizziness happens in about 7% of stapedectomy patients. Taste changes (a metallic or sour taste) affect 4%-usually because a nerve runs near the middle ear. Tinnitus can flare up briefly. These mostly fade.
On the positive side, patient satisfaction is high. At Mass Eye and Ear, 87% of stapedectomy patients said their daily hearing improved significantly. Parents of kids with tubes report 92% satisfaction with infection control.

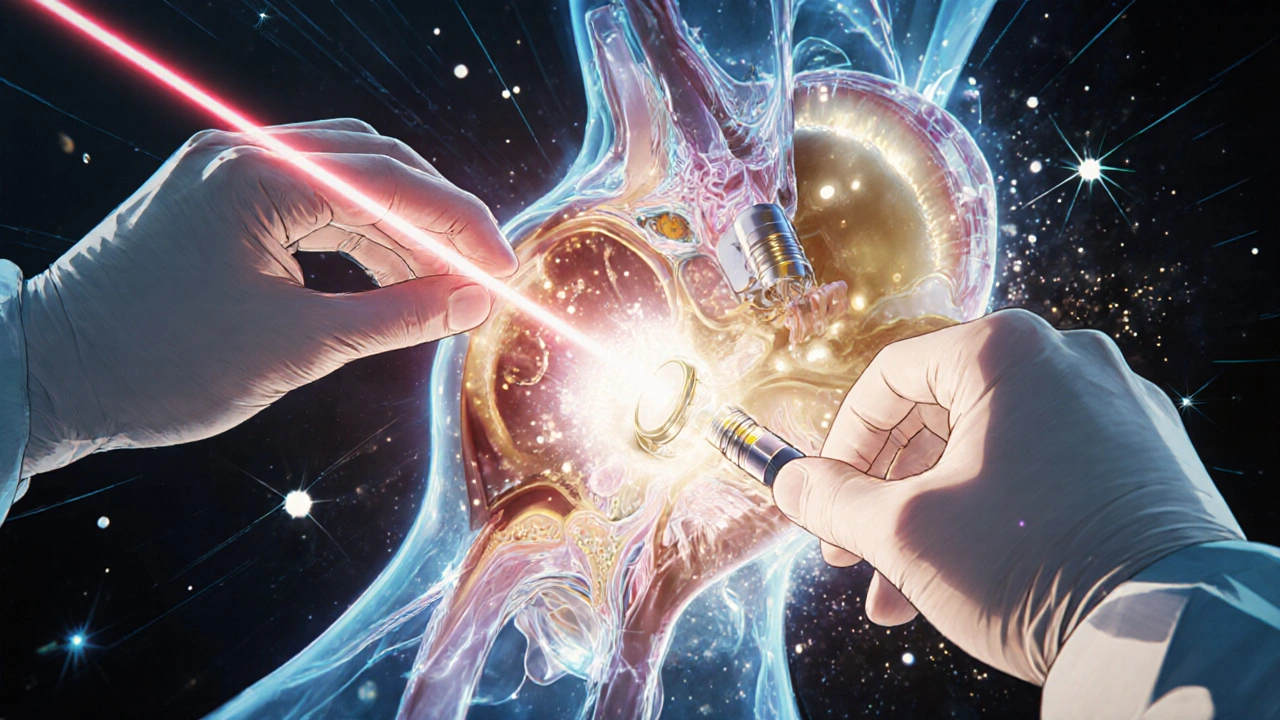
What’s New in Middle Ear Surgery?
Technology is advancing fast. Bioengineered grafts made from extracellular matrix materials are now used in over 30% of tympanoplasties. They have a 92% success rate-better than traditional tissue grafts.
Intraoperative navigation systems, like GPS for the ear, are now in 78% of major ENT practices. They help surgeons avoid nerves and delicate structures during complex cases.
3D-printed ossicular prostheses are in clinical trials. These are custom-made to fit each patient’s anatomy. Early results show 94% hearing improvement-better than standard implants.
Endoscopic surgery, done through the ear canal without an incision, is becoming standard. It gives surgeons a clearer view and reduces recovery time by half. Experts predict it will be used in 60% of procedures by 2028.
When Surgery Isn’t the Answer
Not everyone needs surgery. If your hearing loss is mild, or caused by earwax or a temporary infection, medical treatment is enough. Hearing aids can help too-especially for people who aren’t surgical candidates.
But if you’ve had persistent hearing loss for months, and tests show a clear structural issue, surgery is your best shot at restoring natural hearing. It’s not risky anymore. With modern techniques, it’s safer and more effective than ever.
Next Steps
If you or your child has been told you have conductive hearing loss, don’t wait. Get a full audiological evaluation. Ask for a CT scan if structural damage is suspected. Talk to an otolaryngologist who specializes in middle ear surgery-not just any ENT. Ask about success rates for your specific condition. And don’t be afraid to get a second opinion.
Conductive hearing loss isn’t a life sentence. For most people, it’s a solvable problem. And with today’s technology, hearing can come back-clearly, naturally, and permanently.
Can conductive hearing loss fix itself?
Yes, in some cases. Fluid in the middle ear (glue ear) often clears on its own within 3 months, especially in children. Earwax blockages can be removed easily. But structural issues like otosclerosis, cholesteatomas, or eardrum perforations won’t heal without intervention. If hearing loss lasts more than 3-4 months, medical or surgical treatment is usually needed.
Is surgery for conductive hearing loss safe?
Modern middle ear surgeries are very safe. Complication rates for stapedectomy are now under 2% thanks to laser techniques and better imaging. Tympanoplasty has a 90% success rate for small perforations. Risks include temporary dizziness, taste changes, or tinnitus-but these are rare and usually short-lived. Serious complications like permanent hearing loss occur in less than 1% of cases.
How long does recovery take after ear surgery?
Recovery varies by procedure. For tympanoplasty or stapedectomy, you’ll need 6-8 weeks to fully heal. You can’t get water in your ear, fly, or lift heavy objects during this time. Cholesteatoma surgery may take 4-6 weeks before returning to normal activities. Most people notice improved hearing within 2-4 weeks, but full results take up to 6 months as the ear finishes healing.
Will I need hearing aids after surgery?
Most people don’t need hearing aids after successful middle ear surgery. The goal is to restore natural hearing. But in some cases-like if the inner ear is also affected, or if surgery can’t fully reconstruct the ossicles-hearing aids may still be recommended. Bone-conduction devices are often used for children with aural atresia who aren’t candidates for canal surgery.
Can children have middle ear surgery?
Yes, and it’s very common. Tympanostomy tubes are the most frequent pediatric surgery in the U.S., with over 667,000 done yearly. Canalplasty for aural atresia and tympanoplasty for perforations are also performed in children. Surgery is only recommended if hearing loss affects speech development or if infections are frequent and persistent. Most kids recover quickly and show big improvements in language and learning.
What’s the difference between conductive and sensorineural hearing loss?
Conductive hearing loss means sound can’t reach the inner ear because of a blockage or damage in the outer or middle ear-like wax, fluid, or a broken bone. Sensorineural hearing loss means the inner ear or auditory nerve is damaged-often from aging, noise, or genetics. Conductive loss often improves with surgery or medical treatment. Sensorineural loss is usually permanent and managed with hearing aids or implants.
How do I know if I need surgery?
If your hearing loss is persistent (over 3-4 months), worsens over time, or is confirmed to be conductive with an air-bone gap on audiometry, surgery may be an option. If you have a cholesteatoma, surgery is urgent. If you have frequent ear infections or fluid that doesn’t clear, tubes may help. Always get a full evaluation by an audiologist and an ear specialist before deciding.




Nicole M
November 13, 2025 AT 08:34I had glue ear as a kid and forgot how much it sucked until my nephew got tubes last year. Watching him finally hear his mom say 'I love you' clearly after months of muffled voices? Priceless.
Alex Ramos
November 15, 2025 AT 05:56Just had a stapedotomy last month. The first time I heard birds outside my window without cranking the TV? Tears. Seriously. Recovery was a grind but 100% worth it. Don't let fear stop you if your doc says go for it.
Arpita Shukla
November 16, 2025 AT 06:02Most people don't realize otosclerosis is hereditary. My mom had it, my sister has it, and now I'm being monitored. It's not just 'getting old'-it's a genetic thing that hits women harder. CT scans are non-negotiable. Skip the cheap audiogram at CVS and go straight to a specialist.
Benjamin Stöffler
November 18, 2025 AT 00:22Let’s be honest: modern medicine is a paradox. We can 3D-print ossicles with 94% efficacy, yet insurance still denies coverage for tympanoplasty unless you’re deaf in one ear and crying in a Walmart parking lot. We’ve mastered the anatomy of the ear-but still can’t master the anatomy of healthcare policy.
Mark Rutkowski
November 18, 2025 AT 12:34There’s something profoundly human about hearing your own voice again-not as a hollow echo, but as a real, resonant thing. It’s not just about sound; it’s about rejoining the world. Surgery doesn’t just fix bones-it restores dignity. And that’s why these procedures matter more than most people realize.
Ryan Everhart
November 20, 2025 AT 11:04So you’re telling me we’ve got laser-guided ear surgery and bioengineered grafts… but you still can’t get a decent cup of coffee before 9am? Priorities, people.
manish kumar
November 22, 2025 AT 10:43I’m from India and we don’t have access to this level of care in most towns. My cousin had a cholesteatoma and waited two years because the nearest ENT was 500km away. When he finally got surgery, the doctor had to use a graft from his own thigh because they didn’t have bioengineered material. We need more awareness and better infrastructure-this isn’t just a medical issue, it’s a social justice issue.
Most kids here grow up with untreated glue ear, fall behind in school, and nobody bats an eye. We talk about tech advances in the US but ignore the fact that 70% of the world’s population can’t even get a basic audiogram. It’s not just about fixing ears-it’s about fixing systems.
My brother-in-law got tubes in his 40s after 15 years of hearing loss. He cried when he heard his daughter’s laugh for the first time. That’s the real win-not the success rate numbers, but the quiet moments that come after.
And yes, the CT scans cost a fortune, but if you’re lucky enough to live near a teaching hospital, ask about research trials. I got mine for free through a university program. Don’t assume it’s out of reach.
Also, stop Googling ‘ear surgery horror stories.’ Most of them are from 1995. Modern techniques are safe. The risk of permanent hearing loss is less than 1%. You’re more likely to die from a banana peel than from a stapedotomy.
And for the love of God, if you’re a parent and your kid keeps asking ‘what?’ three times in a row, don’t just blame the TV. Get them checked. Speech delays from untreated conductive loss are irreversible after age 5.
I’ve seen too many kids grow up thinking they’re ‘slow’ when they just couldn’t hear the teacher. It’s not their fault. It’s our failure to act.
So if you’re reading this and you’ve been putting off an appointment-do it. Not for the surgery. For the silence that comes after the noise stops.
David Barry
November 23, 2025 AT 17:53Let’s not romanticize this. 87% satisfaction? That means 13% are still miserable. And 4% get taste changes? That’s not ‘rare’-that’s one in twenty people losing their ability to enjoy food. And you call that ‘minor’? This isn’t a cosmetic procedure. It’s a gamble with your senses.
Also, 3D-printed implants? Cool. But who pays for it? And what happens when the prosthesis fails in 10 years? You think they’ll just reprint it for free? Welcome to the future of medicine-expensive, fragile, and built on corporate patents.
Alyssa Lopez
November 25, 2025 AT 17:05Y’all are overthinking this. Just get the tubes. My cousin had 5 ear infections in 6 months. Doc put in tubes. Done. No drama. No 3D printing. Just a lil’ hole and boom-no more pain. Stop reading all this sci-fi stuff and just go see an ENT. Jargon doesn’t fix ears.
edgar popa
November 26, 2025 AT 19:48Got my stapedotomy in March. Hearing my dog bark clearly for the first time? Best day ever. Recovery sucked but worth every second. Don’t wait.
Eve Miller
November 26, 2025 AT 22:59It’s irresponsible to suggest that ‘surgery is safe’ without emphasizing the absolute necessity of preoperative counseling, informed consent documentation, and postoperative audiometric follow-up protocols. The article glosses over the ethical obligation to disclose all potential risks, including facial nerve injury and perilymph fistula, which, while rare, are not negligible. This is not a trivial procedure.
Chrisna Bronkhorst
November 27, 2025 AT 07:25Conductive loss? Yeah, I had it. Got the surgery. Heard better. Then my insurance raised my rates because I ‘used a covered benefit.’ Welcome to America. Fix the system before you fix my ear.