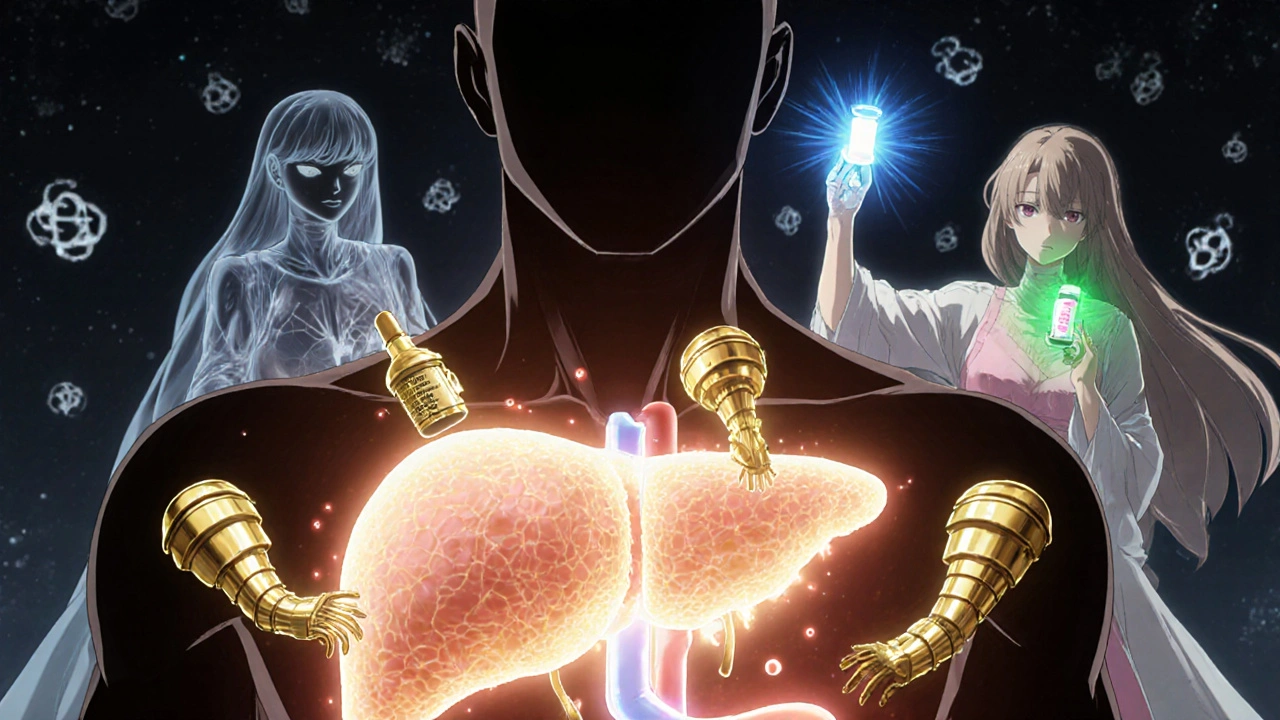
What Is Autoimmune Hepatitis?
Autoimmune hepatitis (AIH) is a chronic liver disease where your immune system mistakenly attacks your own liver cells. It’s not caused by alcohol, viruses like hepatitis B or C, or fatty liver. Instead, your body turns against itself, triggering inflammation that can slowly destroy liver tissue. Left untreated, it can lead to cirrhosis, liver failure, or the need for a transplant.
First identified in the 1950s as "lupoid hepatitis," AIH was later recognized as a distinct condition when doctors noticed patients responded dramatically to immune-suppressing drugs. Today, it affects about 10 to 25 people per 100,000 worldwide, with women making up roughly 80% of cases. It can show up at any age, but peaks in your 20s and 60s.
How Is Autoimmune Hepatitis Diagnosed?
There’s no single test for AIH. Diagnosis requires putting together pieces from blood work, liver biopsy, and ruling out other causes. Blood tests usually show high levels of liver enzymes - ALT and AST - often five to ten times above normal. Immunoglobulin G (IgG), a type of antibody, is also typically elevated by more than 1.5 times the upper limit.
Autoantibodies are key clues. Most patients (about 80%) test positive for antinuclear antibodies (ANA) or smooth muscle antibodies (SMA). A smaller group has liver-kidney microsomal type 1 antibodies (LKM1). But here’s the important part: the type of antibody doesn’t change how you’re treated. The 2025 European Association for the Study of the Liver (EASL) guidelines stopped recommending subclassification because it didn’t affect outcomes.
The gold standard for diagnosis is a liver biopsy. A small sample of liver tissue is taken using a thin needle, guided by ultrasound. The pathologist looks for "interface hepatitis" - inflammation right where the liver’s portal areas meet the main tissue. This pattern is almost unique to AIH. Biopsies need at least 20 portal tracts to be reliable. The risk of serious complications like bleeding is very low - under 0.3%.
Doctors use the Revised International Autoimmune Hepatitis Group (IAIHG) scoring system to help confirm the diagnosis. Points are given for symptoms, blood markers, biopsy findings, and exclusion of other diseases. A score above 15 suggests probable AIH; above 20 means definite AIH.
Why Steroids Are the First Step in Treatment
Once AIH is confirmed, treatment starts with a corticosteroid - usually prednisone or prednisolone. These drugs calm down the overactive immune system. Within two weeks, most patients see their liver enzymes drop significantly. That rapid response is actually a diagnostic clue in itself.
Initial dosing is typically 0.5 to 1 mg per kilogram of body weight per day, capped at 60 mg daily. For someone weighing 70 kg, that’s around 35 to 70 mg per day. The goal isn’t to stay on this dose forever. Doctors aim to taper it down over 6 to 8 weeks to a maintenance level of 10 to 15 mg daily.
But steroids come with a cost. About 70% of people on steroid-only treatment develop side effects. These include weight gain, "moon face," fluid retention, mood swings, insomnia, high blood sugar, bone thinning, and cataracts. One patient on Reddit described gaining 30 pounds of fluid in three weeks. Another said they looked "unrecognizable." These aren’t rare - they’re expected.

How Azathioprine Helps - and Why It’s Used With Steroids
Azathioprine (brand names: Imuran, Azasan) is an immunosuppressant that’s been used alongside steroids since the 1970s. It doesn’t work as fast as steroids, but it lets doctors cut the steroid dose by 70 to 80% within six months. That’s huge for reducing side effects.
The standard starting dose is 50 mg per day, then slowly increased to 1 to 2 mg per kg per day - up to 150 mg daily. It’s usually started at the same time as steroids or within the first few weeks.
But azathioprine isn’t risk-free. About 35% of patients get stomach upset, nausea, or diarrhea. In 12% of cases, it lowers white blood cell counts, increasing infection risk. Rarely, it can cause pancreatitis - one patient on the American Liver Foundation forum had to stop azathioprine after it triggered severe pancreatitis at 100 mg.
That’s why testing for TPMT enzyme levels is now standard before starting azathioprine. About 0.3% of people have a complete deficiency in this enzyme. If they take azathioprine, they face a 30-fold higher risk of life-threatening bone marrow suppression. Testing costs $250 to $400 in the U.S., and while 89% of U.S. academic centers now do it, only 45% of smaller clinics still skip it.
What Does Successful Treatment Look Like?
Success isn’t just about feeling better. It’s measured by blood tests and, eventually, a second liver biopsy.
A complete biochemical response means ALT and AST return to normal, and IgG levels drop back to normal. This happens in 60 to 80% of patients within 18 to 24 months. But it takes time. The 2025 EASL guidelines moved away from checking response at 6 months - many patients need 6 to 12 months to show real improvement.
When liver inflammation fades, fibrosis can actually reverse. One patient shared on HealthUnlocked that after two years on low-dose steroids and azathioprine, their biopsy went from F3 (advanced scarring) to F0 (no scarring). That’s not just stabilization - that’s healing.
But treatment isn’t over when labs normalize. Most patients (60 to 80%) need to stay on low-dose maintenance therapy indefinitely. Stopping too soon leads to relapse in 50 to 90% of cases. Even after years of remission, 70% of relapses happen within three months of stopping medication.

What If Treatment Doesn’t Work?
For 10 to 15% of patients, steroids and azathioprine don’t control the disease. This is called treatment failure. Signs include ALT and AST staying above twice the upper limit after 12 to 18 months.
When that happens, doctors turn to second-line drugs. Mycophenolate mofetil (CellCept) is the most common. It’s dosed at 1 to 1.5 grams twice daily and works well for patients who can’t tolerate azathioprine. About 60% of non-responders improve on this drug.
Other options include calcineurin inhibitors like tacrolimus or cyclosporine. These are powerful but carry risks of kidney damage and high blood pressure. They’re usually reserved for complex cases.
Emerging therapies are on the horizon. JAK inhibitors like tofacitinib are showing 55% response rates in early trials. Monoclonal antibodies targeting IL-6, like clazakizumab, have achieved 50% complete response in phase 2 studies. Obeticholic acid (Ocaliva), originally for primary biliary cholangitis, is now in phase 3 trials for AIH and showed a 42% response rate in 2024.
What You Need to Know Before Starting Treatment
Before any immunosuppressant is started, you must be tested for hepatitis B. About 15 to 20% of people carry hidden hepatitis B virus (HBV). Immunosuppressants can wake it up, causing severe liver damage. If you test positive for HBsAg or anti-HBc, you’ll need antiviral prophylaxis - usually tenofovir - before starting steroids or azathioprine.
Vaccinations matter too. Get hepatitis A and B shots before treatment begins. Once you’re on immunosuppressants, vaccines work much less well - only 40 to 60% effective versus 90% in healthy people.
Monitoring is non-negotiable. Blood tests every 2 to 4 weeks during the first few months, then every 3 months. IgG levels checked quarterly. A repeat biopsy is recommended after 18 to 24 months to confirm histological remission - not just biochemical improvement.
Living With AIH: Real Challenges and Real Hope
AIH is a lifelong condition. It’s not curable, but it’s manageable. The biggest hurdle isn’t the disease - it’s the treatment. Patients report steroid side effects as worse than the symptoms of the disease itself. Weight gain, mood swings, and fatigue take a heavy toll.
But the story isn’t all bleak. With consistent treatment, most people live normal lives. Liver function stabilizes. Fibrosis reverses. Many return to work, travel, and raise families.
The future is promising. Research is moving toward personalized medicine. Genetic markers like HLA-DRB1*03:01 and *04:01 help predict who’s likely to have severe disease. Blood tests for microRNA are being tested to predict steroid response within two weeks - potentially avoiding months of trial and error.
And awareness is growing. The Autoimmune Hepatitis Association has seen 20% annual membership growth since 2020. More doctors are using the latest guidelines. More patients are speaking up. You’re not alone.
Can autoimmune hepatitis be cured?
No, autoimmune hepatitis cannot be cured, but it can be controlled. With proper treatment, most patients achieve long-term remission, where liver inflammation stops and damage halts or even reverses. Many stay on low-dose medication for life to prevent relapse. Stopping treatment too soon leads to relapse in 50 to 90% of cases.
How long do you take steroids for autoimmune hepatitis?
Steroids are started at a high dose and tapered over 6 to 8 weeks to a maintenance level of 10 to 15 mg daily. Most patients stay on this low dose for years - often for life. The goal is to combine steroids with azathioprine so the steroid dose can be reduced as much as possible. Some patients eventually stop steroids entirely if azathioprine keeps the disease under control.
Does azathioprine cause weight gain?
No, azathioprine does not typically cause weight gain. That’s a side effect of steroids like prednisone. Azathioprine is more likely to cause nausea, fatigue, or low blood cell counts. Some patients report hair thinning or mild stomach upset. Weight gain is almost always tied to steroid use, not azathioprine.
Can you drink alcohol with autoimmune hepatitis?
No. Alcohol puts extra stress on an already inflamed liver. Even small amounts can speed up scarring and increase the risk of cirrhosis. Doctors strongly recommend complete abstinence from alcohol for all patients with autoimmune hepatitis, regardless of disease activity.
Is a liver biopsy always necessary?
Yes, a liver biopsy is required for a definitive diagnosis. Blood tests and antibodies can suggest AIH, but only a biopsy can confirm the specific pattern of liver damage - interface hepatitis - that makes the diagnosis certain. It’s also used later to check if treatment is working and if fibrosis is improving.
What happens if I miss a dose of azathioprine?
If you miss one dose, take it as soon as you remember that day. If it’s almost time for your next dose, skip the missed one and continue your regular schedule. Do not double up. Missing doses increases the risk of relapse. If you miss several doses, contact your doctor - you may need blood tests to check liver enzymes and blood counts before restarting.




Karla Luis
November 26, 2025 AT 08:20Kenneth Narvaez
November 27, 2025 AT 16:26jon sanctus
November 27, 2025 AT 20:52Matt Webster
November 28, 2025 AT 17:28Sharmita Datta
November 28, 2025 AT 19:34mona gabriel
November 29, 2025 AT 11:32jeff melvin
November 29, 2025 AT 14:39Fiona Hoxhaj
December 1, 2025 AT 00:15Phillip Gerringer
December 1, 2025 AT 01:35Stephen Wark
December 1, 2025 AT 09:49Liliana Lawrence
December 1, 2025 AT 13:26Christian Mutti
December 3, 2025 AT 07:15Hamza Asghar
December 3, 2025 AT 12:26Jaylen Baker
December 4, 2025 AT 15:49Daniel McKnight
December 6, 2025 AT 08:29