When someone suddenly can’t breathe, their skin breaks out in hives, and their throat feels like it’s closing, time isn’t just important-it’s everything. This isn’t a panic attack. It’s anaphylaxis, a life-threatening allergic reaction that can turn normal into deadly in under a minute. And the only thing that can stop it? Epinephrine. No ifs, no maybes. If you or someone you care about has a severe allergy, this isn’t just information-it’s a survival guide.
What Exactly Is Anaphylaxis?
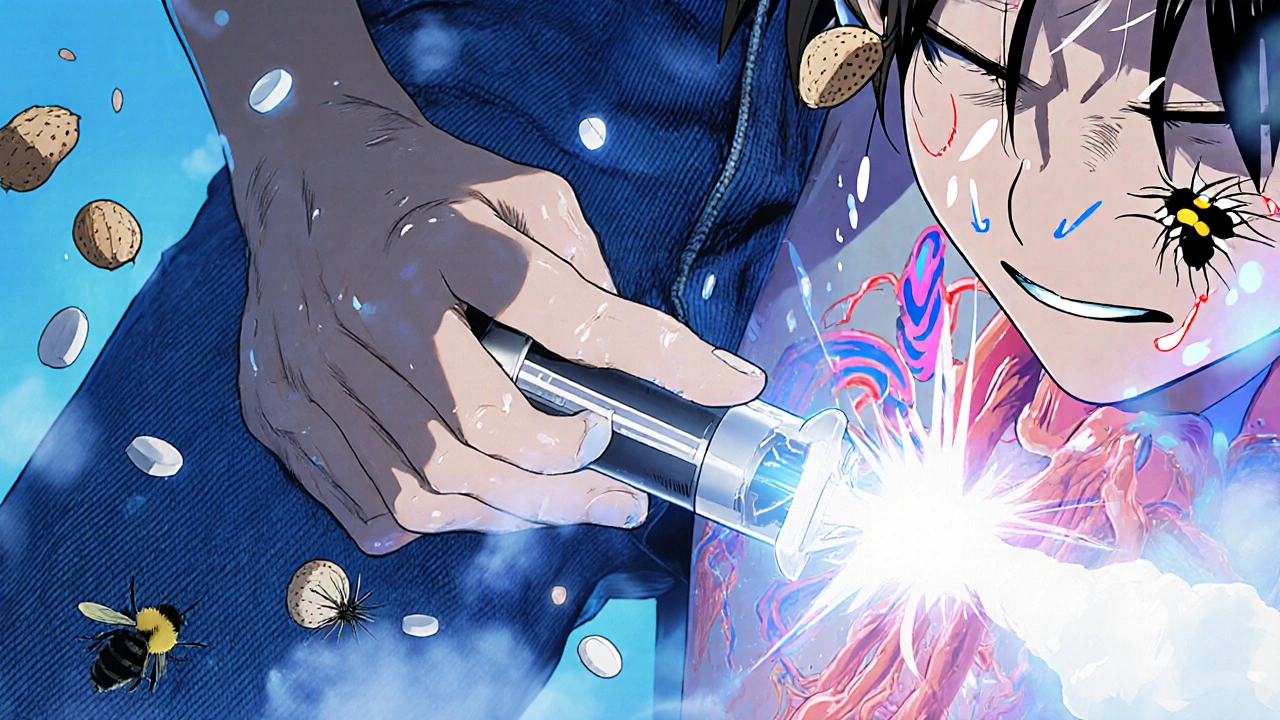
Anaphylaxis isn’t just a bad rash or a stuffy nose. It’s your immune system going into overdrive, releasing chemicals that crash your blood pressure, swell your airways, and shut down your body’s ability to breathe. It doesn’t wait for permission. It doesn’t ask if you’re ready. It hits fast-usually within minutes of exposure to an allergen-and it can kill if not treated immediately. The signs aren’t always obvious at first. You might see a few hives or swelling around the lips. Then comes the wheezing, the dizziness, the nausea. Some people feel like they’re going to pass out. Others vomit or have stomach cramps. These aren’t random symptoms-they’re the body screaming for help. According to the Resuscitation Council UK, anaphylaxis is diagnosed when you have acute symptoms affecting the skin and either breathing problems or low blood pressure. That’s the rule. No gray area. Common triggers? Foods like peanuts, tree nuts, shellfish, and eggs. Insect stings from bees or wasps. Medications like penicillin. Even latex can do it. And here’s the scary part: you don’t need to eat a whole peanut to trigger it. A crumb, a whiff of steam from cooking shrimp, or a touch of residue on a fork can be enough.Why Epinephrine Is the Only Thing That Works
You’ve probably heard people say, “Just take an antihistamine.” Don’t. Not when it’s anaphylaxis. Antihistamines like Benadryl might help with a mild rash, but they do absolutely nothing to stop airway swelling or restore blood pressure. A Cochrane review from 2012 found zero evidence that antihistamines alone save lives in anaphylaxis. Corticosteroids? They might help prevent a second wave of symptoms hours later, but they’re useless in the first 10 minutes. Epinephrine is the only treatment that directly reverses the dangerous changes in your body. It tightens blood vessels to raise blood pressure, opens up your airways so you can breathe, and stops the release of more dangerous chemicals. It works fast-within minutes. Studies show 85% of people improve within five minutes if they get epinephrine right away. If you wait? That number drops to 42%. It’s not magic. It’s science. Epinephrine activates alpha and beta receptors in your body. Alpha receptors constrict blood vessels. Beta receptors relax your lungs. Together, they buy you the time you need to get to a hospital. And yes, you still need to call 911 after using it. But without epinephrine, you won’t make it to the hospital.How to Use an Epinephrine Auto-Injector
There are three main brands in Australia and the U.S.: EpiPen, Auvi-Q, and Adrenaclick. They all work the same way, but the design differs. The key is to know yours. Here’s the simple, step-by-step process:- Remove the safety cap.
- Place the tip firmly against the outer thigh-through clothing if needed.
- Push hard until you hear a click. Hold it in place for 3 seconds.
- Remove and massage the area for 10 seconds.
- Call emergency services immediately-even if you feel better.
Why People Wait-And Why That’s Deadly
The biggest killer in anaphylaxis isn’t the reaction itself. It’s delay. A 2020 study in the Journal of Allergy and Clinical Immunology found that 43% of people wait too long before using epinephrine. Why? They think it’s “just a rash.” Or they’re afraid of the needle. Or they believe antihistamines will be enough. Some parents wait to see if their child gets worse before acting. That’s the mistake. Dr. Maria Garcia-Lloret from UCLA says it plainly: “Delaying epinephrine is the single greatest predictor of poor outcomes.” And she’s right. In emergency rooms across the U.S., over half of patients who clearly meet anaphylaxis criteria never get epinephrine before being admitted. That’s not a failure of medicine-it’s a failure of awareness. Even trained people get it wrong. A 2021 study showed 68% of people using auto-injectors in simulations did it incorrectly-wrong placement, not holding long enough, forgetting to call for help. Practice matters. Buy a training device. Use it once a month. Get your family to practice too.Cost, Access, and Keeping Your Injector Ready
Epinephrine auto-injectors cost money. In Australia, they’re subsidized through the PBS, but in the U.S., prices still hover around $300-$650 for a two-pack. Generic versions are now available and cover 70% of prescriptions, bringing prices down. But even then, 30% of people can’t afford to refill them regularly. Store your injector at room temperature. Don’t leave it in the car. Don’t put it in the fridge. Extreme heat or cold can break it down. Check the expiration date every month. The liquid inside should be clear. If it’s brown or cloudy, replace it. And here’s a tip most people miss: keep two. Always. Anaphylaxis can come back hours later-a “biphasic reaction.” You might feel fine after the first shot, then crash again. Having a second injector ready isn’t paranoia. It’s standard care.
What Comes After the Injection
Using epinephrine isn’t the end. It’s the beginning of the next step: hospital care. Even if you feel better, you need to be observed for at least 4-6 hours. Some patients-especially those with asthma or heart conditions-need 12 hours. Why? Because the reaction can return. And without monitoring, you could slip into shock while thinking you’re safe. Emergency teams will give you more epinephrine if needed, along with oxygen, IV fluids, and steroids. But none of that replaces the first shot you gave yourself. After discharge, you should get a written action plan. Not a vague note. A clear, step-by-step document that says: “If these symptoms happen, do this.” If your doctor doesn’t give you one, ask for it. And make sure your school, workplace, or daycare has a stock injector on hand. In the U.S., all 50 states now require schools to keep them. Australia is catching up.The Future: New Tools and Better Access
In August 2023, the FDA approved Neffy-a nasal spray version of epinephrine. No needle. Just spray into one nostril. It’s not for everyone (it’s not as fast as the injection), but for people terrified of needles, it’s a game-changer. New smart injectors are in testing. One prototype connects to your phone and sends a text to your emergency contacts the moment it’s used. Others have built-in reminders for expiration dates. And research into drugs like omalizumab (Xolair) shows promise for reducing how often people need epinephrine in the first place. But none of this replaces the basics: know the signs. Carry the injector. Use it early. Call for help. Practice. Teach others.Final Thought: This Isn’t About Fear. It’s About Preparedness.
Anaphylaxis isn’t rare. About 1 in 50 people in Australia and the U.S. have experienced it. Food allergies alone have tripled in kids over the last 20 years. The world is more allergic than ever. But here’s the good news: anaphylaxis is preventable in death. With epinephrine, it’s survivable. You don’t need to live in fear. You just need to be ready. If you have a severe allergy, carry your injector. If you’re the parent of a child with one, make sure everyone who watches them knows how to use it. If you’re a teacher, a coach, or a friend-learn what to do. Because when seconds count, the only thing that matters is that someone knows how to act.Can antihistamines stop anaphylaxis?
No. Antihistamines like Benadryl may help with mild itching or hives, but they do nothing to reverse airway swelling, low blood pressure, or shock-the real dangers of anaphylaxis. Relying on them instead of epinephrine can be fatal. Epinephrine is the only treatment proven to save lives during an acute reaction.
How do I know when to use my epinephrine injector?
Use it at the first sign of a serious reaction: trouble breathing, swelling of the tongue or throat, dizziness, rapid pulse, or a combination of skin symptoms (hives, flushing) and gastrointestinal issues (vomiting, cramps). Don’t wait for collapse. Don’t wait to confirm. If you suspect anaphylaxis, inject immediately. Delaying is the most common reason for poor outcomes.
Can I use someone else’s epinephrine injector?
Yes. If you’re helping someone having anaphylaxis and they don’t have their own injector, use yours. Epinephrine is safe even if given to someone without an allergy. The risk of not using it far outweighs any possible side effects. There’s no legal or medical barrier to using another person’s injector in an emergency.
Do I need to go to the hospital after using epinephrine?
Absolutely. Even if you feel better, you need to be monitored for at least 4-6 hours. Anaphylaxis can return hours later in what’s called a biphasic reaction. Emergency teams can give you additional treatment, monitor your breathing and blood pressure, and make sure you’re stable before you go home.
How often should I replace my epinephrine injector?
Check the expiration date on the side of the injector. Most last 12-18 months. Replace it before it expires. Even if the liquid looks clear, the medication can lose potency over time. Don’t wait until it’s expired to refill. Keep two on hand at all times-one for backup.
Is there a needle-free option for epinephrine?
Yes. Neffy, a nasal spray version of epinephrine, was approved by the FDA in August 2023. It’s designed for people who fear needles or have trouble using injectors. It’s not as fast as an injection, but it’s a valuable alternative. In Australia, it’s still under review and not yet available. Always have an injector as your first-line option unless your doctor advises otherwise.





Ravi Kumar Gupta
November 22, 2025 AT 16:24Bro, I saw this happen in Delhi last year - guy ate a samosa with trace peanut oil, went down in 90 seconds. Bystanders were panicking, no epinephrine in sight. His wife screamed for someone to call an ambulance, but no one knew what to do. I grabbed his EpiPen from his bag - he’d told me about it last Diwali - and used it. He was breathing again in 2 minutes. Don’t wait. Don’t overthink. Just inject.
India needs more public awareness. Schools, trains, temples - they should have stock injectors. This isn’t just a Western problem.
Epinephrine isn’t scary. Not using it is.
Rahul Kanakarajan
November 23, 2025 AT 08:38Ugh. Another one of these fear-mongering articles. You people act like every little rash is the end of the world. I’ve had hives from spicy food my whole life and I’m still standing. Antihistamines work fine for most people. Stop scaring folks into buying expensive pens just so you can profit off their anxiety.
And why is everyone suddenly obsessed with epinephrine like it’s holy water? It’s just adrenaline. You think your body can’t handle a little allergic reaction? Grow up.
New Yorkers
November 23, 2025 AT 21:36Look. I live in NYC. I’ve seen people go down on the subway from a peanut butter sandwich. I’ve seen parents cry because they didn’t know how to use the pen. I’ve seen EMTs show up and say ‘we didn’t bring enough epinephrine.’
This isn’t hyperbole. This is reality. You think you’re being tough by saying ‘it’s just a rash’? That’s the same logic that got people killed in the early AIDS crisis. Denial doesn’t save lives. Action does.
And if you’re too lazy to learn how to use a pen - don’t blame the article. Blame yourself.
Also - Neffy is a game changer. I’m not scared of needles anymore. And I’m not dying because of it.
David Cunningham
November 25, 2025 AT 08:44Been there. My niece had her first reaction at a birthday party in Melbourne. Cake had trace nuts. She broke out in hives, started wheezing. Her dad grabbed the EpiPen - but used it on her arm. Took 10 minutes to get to hospital. She’s fine now, but it was close.
Point is - it’s not just about having it. It’s about knowing how to use it. And telling everyone around you. Teachers, coaches, grandparents. My sister now keeps two in the car, one at school, one at home. No excuses.
And yeah - the cost sucks. But if you can afford a phone, you can afford a refill. It’s not optional.
luke young
November 25, 2025 AT 19:55Love this post. So clear, so urgent. I’m a teacher and I just got trained on using the school’s stock injector last week. I didn’t realize how much I didn’t know - like how you can use someone else’s pen if needed. That’s huge.
My kid has a dairy allergy, not peanuts, but now I get it - it’s not about the allergen, it’s about the reaction. And speed. I’m printing out the steps and taping them to the fridge. My wife and I are doing monthly drills with the trainer pen. No more hoping for the best.
Thanks for making this feel less scary and more doable.
james lucas
November 26, 2025 AT 17:43so i just wanna say i had no idea epinephrine was that simple to use like i always thought you needed to be a doctor or something but nope just push and hold for 3 seconds?? wow. and the part about the second dose?? i mean i always thought if you used it once you were done but nope you can do it again if it doesnt work?? like that’s wild. and the brown liquid thing?? i’ve had mine for 18 months and it still looks clear but i never checked the date. gonna go check right now. also i just bought my second one because i was scared of running out. my mom says i’m overreacting but honestly i’d rather be annoying than dead. also can we just talk about how no one ever teaches you this in school?? like we learn how to do long division but not how to save a life?? crazy.
Jessica Correa
November 27, 2025 AT 07:11I used to think antihistamines were enough until my cousin went into shock at a BBQ. She took Benadryl and sat down. Thought she’d be fine. Took 20 minutes for someone to realize she wasn’t breathing. She’s okay now but it took three doses of epinephrine in the ER. I carry two now. Always. I don’t care if I look paranoid. I’d rather look weird than lose someone.
Also the nasal spray thing? I’m so excited. I hate needles. I’ve been avoiding getting one because of it. If Neffy works even half as good, I’m switching.
manish chaturvedi
November 28, 2025 AT 22:24As someone who grew up in a household where allergies were dismissed as ‘weakness,’ I am deeply moved by this article. In many parts of India, allergic reactions are still misunderstood as psychosomatic or exaggerated. We must change this narrative.
Epinephrine is not a luxury - it is a right. Every public institution, every school, every temple and train station should have at least one auto-injector available and staff trained to use it. This is not merely medical advice - it is public health infrastructure.
Let us not wait for another tragedy to act. Let us act now - with compassion, with clarity, and with courage.
Nikhil Chaurasia
November 29, 2025 AT 10:28I’ve never had anaphylaxis. But I’ve seen my cousin go through it. He didn’t want to carry the pen because he was embarrassed. Said people would stare. Said it made him feel ‘broken.’
I didn’t say anything then. But now I tell everyone - you’re not broken. You’re prepared. And that’s powerful.
I keep two in my backpack. One for me. One for anyone who needs it. No questions. No judgment. Just life.
Holly Schumacher
December 1, 2025 AT 03:57Let me correct a few things. The Cochrane review you cited is from 2012 - outdated. A 2021 meta-analysis in JACI showed antihistamines may have a *modest* effect on cutaneous symptoms, but zero effect on mortality. You’re correct about epinephrine, but your phrasing implies it’s the *only* treatment - it’s not. Oxygen, IV fluids, glucagon for beta-blocked patients, and bronchodilators are all part of standard care. You’re oversimplifying.
Also, ‘30% of people can’t afford to refill’ - that’s a systemic failure, not an individual one. Blaming the patient is lazy. The FDA and insurers need to fix pricing. And Neffy? It’s 85% as effective as injection in adults - not ‘game-changing.’ It’s a backup. Don’t mislead people.
And yes - you still need to call 911. But you didn’t mention that epinephrine can cause tachycardia, tremors, anxiety - which may be mistaken for panic. That’s why monitoring matters.
Accuracy matters. Lives depend on it.
Michael Fitzpatrick
December 2, 2025 AT 21:13Man, this hit home. My daughter’s allergic to eggs and dairy - we’ve had a few scary moments. The first time she reacted, I froze. I didn’t know if it was ‘bad enough’ to use the pen. Turned out it was. She’s fine now, but I still wake up sometimes thinking about it.
Since then, we’ve made it a family thing. We do the ‘injector drill’ every Sunday morning. My wife, my mom, even my 7-year-old knows how to hold it and push. We keep one in her backpack, one in the glovebox, one at grandma’s house.
And I’ll be honest - I used to think it was overkill. Now I know it’s not. It’s just responsibility. We don’t live in fear. We live prepared. And that’s the difference.
Also - Neffy sounds amazing. I’m already on the waitlist. No more shaking hands trying to jab a needle into a screaming kid. Please let this become mainstream faster.